How drugs work - Pharmacodynamics
General mechanisms of drug action
1. Acting on specific proteins on cell membranes called receptors
2. Acting in synapses
3. Blocking the action of specific enzymes
4. Inhibiting cell transport mechanisms
5. Acting on invading organisms
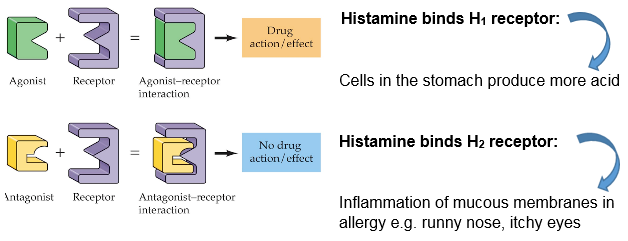
Receptor theory: Histamine as an example
The lock and key concept
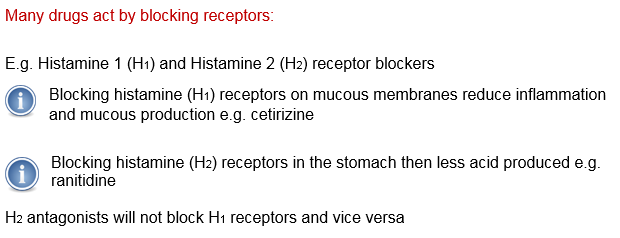
Side effects
Drugs are not always specific some H1 antagonists have weak anticholinergic properties
- dry mouth and dry eyes
Receptors in other areas besides where drug is required to act
- H1 receptors in the brain cause drowsiness
The adrenergic receptor
The effects of adrenaline
- speeds up heart and pumps harder
- constricts arteries and increases blood pressure
- dilates the bronchioles (opens the airways)
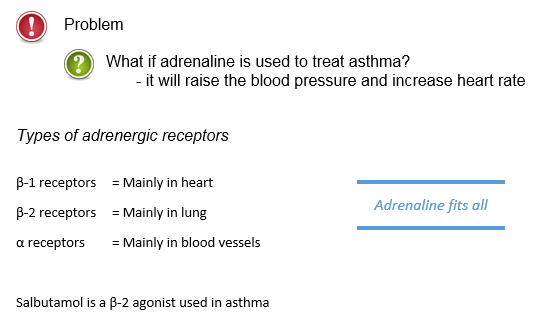
Side effects of ß Blockers
Propranolol blocks ß 1 and ß 2 receptors
- makes asthma worse
Selectivity is only relative
- atenolol blocks ß 1 more than ß 2
- best avoided still in asthma
Most antagonists work by competition
- depends on concentration of agonist v antagonist
Secondary messengers
There are process intermediates between binding on receptor and effect. Example -adrenoreceptors:
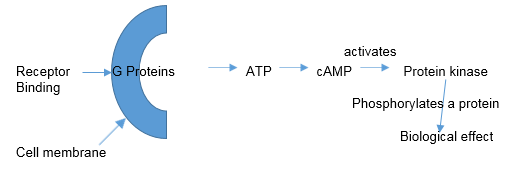
Some drugs do not involve secondary messengers:
Some enter the cells quite easily and the ‘receptor’ is inside the cells e.g. Corticosteroids.
- The glucocorticoid receptor complex enters nucleus
- Binds to DNA has action via mRNA
Insulin binds to receptors directly triggering a response via enzymes
- Increased glucose uptake
- Insulin binds with a receptor subunit (alpha)
- This complex enters the cell where insulin is destroyed
- The binding activates the tyrosine kinase activity of the beta sub unit leading to effect
Drugs that inhibit enzymes
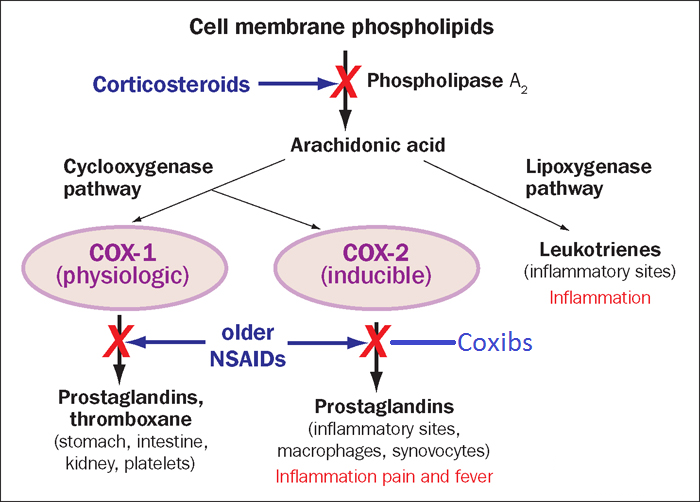
Non-steroidal anti-inflammatories (NSAIDs) inhibit the formation of prostaglandins responsible for modulating inflammation
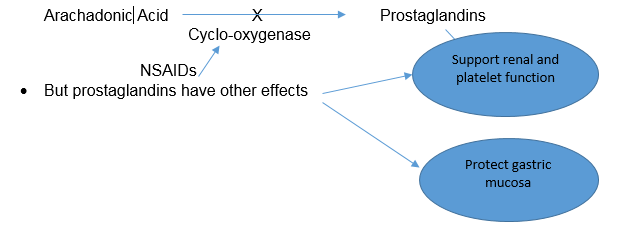
Prostoglandins reduce acid production and increase mucus in stomach as well as increase blood flow to kidneys
We can anticipate side effects of NSAIDs with this
- peptic ulceration
- salt and water retention
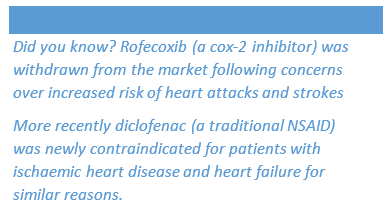
COX-2: A more recent Anti-Inflammatory Drug Target
Drugs that inhibit enzymes
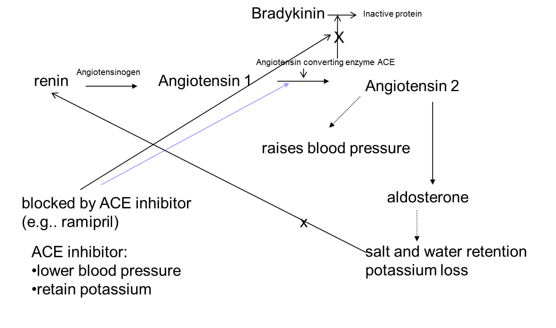
Angiotensin converting enzyme (ACE) inhibitors
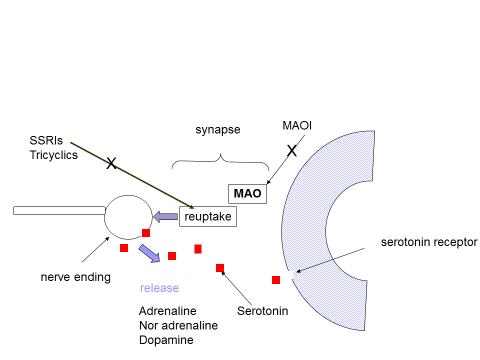
Action in the Nerve Synapse
Proposed action of antidepressant on neurotransmitters
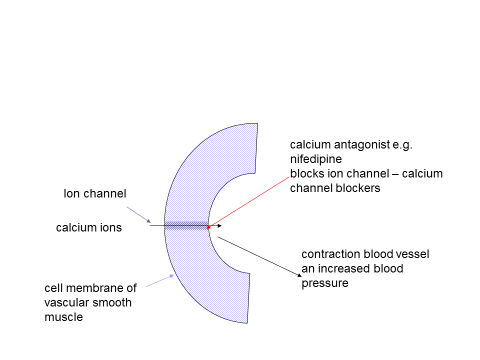
Drugs affecting cell transport
Interfering with the movement of ions across cell membranes
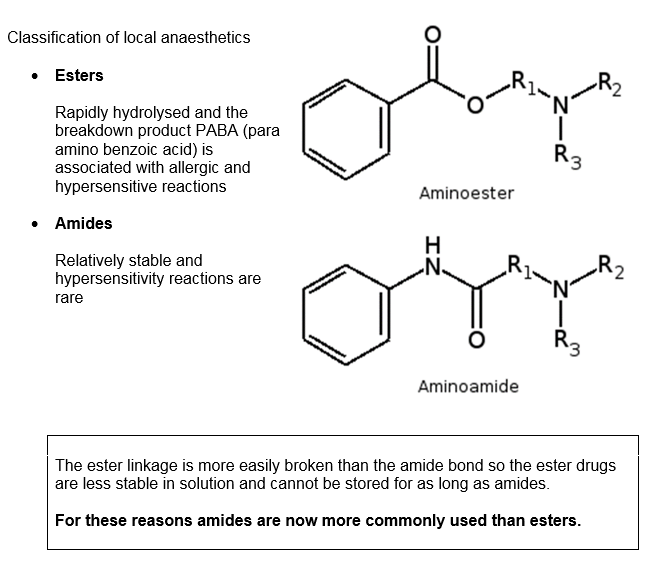
Local Anaesthetics
Local anaesthetics generally have a lipid-soluble hydrophobic aromatic group and a charged, hydrophilic amine group.
The bond between these two groups determines the class of the drug, and may be amide or ester.
Examples of amides include: lignocaine, bupivacaine and prilocaine.
Examples of esters include: cocaine and amethocaine.
Mode of action
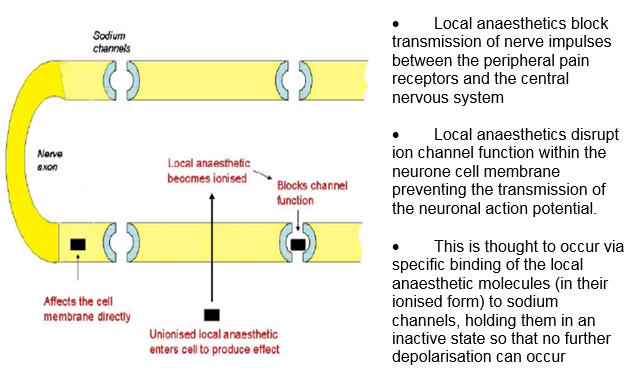
- Local anaesthetics diffuse through the lipophilic nerve membrane unionized
- Low pH in cell generates ionized form
- Ionized LA blocks the channel
- Impulses stopped
- Slowly returns to normal and impulses return as block ends
Factors affecting anaesthetic effect
- Small diameter nerve fibres are more sensitive to local anaesthetics than larger fibres so pain sensation is blocked more readily than touch and movement.
- The action is dose dependent
- The action is pH dependent (inflamed tissues are often acidic and resistant to local anaesthetics)
Adverse effects
- Local anaesthetics block sodium channels in the conduction system of the heart. This can cause myocardial depression and vasodilatation.
- Local anaesthetics can also affect the CNS. Stimulation causes restlessness and at high doses, convulsions
- Addition of adrenaline causes constriction of peripheral blood vessels, lessening the distribution, prolonging action and producing a relatively bloodless field.
Absorption and Distribution
- Local anaesthetic drugs are administered to the areas around the nerves to be blocked – which include skin, subcutaneous tissues, intrathecal and epidural spaces.
- Some of the drug will be absorbed into the systemic circulation
- Most local anaesthetics have vasodilatory effects at low concentrations, increasing their systemic absorption. This is countered in some preparations which include a vasoconstrictor such as adrenaline.
- The distribution of the drug is influenced by the degree of tissue and plasma protein binding of the drug.
- The more protein bound the agent, the longer the duration of action as free drug is more slowly made available for metabolism.
Metabolism and Excretion
- Ester and amide anaesthetics differ in their metabolism.
- Esters (except cocaine) are broken down rapidly by plasma esterases to inactive compounds and consequently have a short half-life.
- Amides are metabolised hepatically by amidases. This is a slower process, hence their half-life is longer and they can accumulate if given in repeated doses or by infusion.
- Prilocaine is also metabolised extra-hepatically.
Newer Agents
- Levobupivacaine (Chirocaine)
- Ropivacaine (Naropin)
- Purified stereoisomers can reduce toxicity
References: http://www.frca.co.uk/article.aspx?articleid=100505
Drugs with a non-specific action
Antacids e.g. aluminum hydroxide
- neutralise acid in stomach
Emollients
- moisturise skin
General anaesthetics
- reduce CNS function
Mode of action of antimicrobials
Beta Lactam antibiotics e.g. Penicillins
- inhibit bacterial cell wall synthesis
Macrolides e.g. erythromycin
- inhibit bacterial protein synthesis
Antifungal agents e.g. nystatin
- inhibit ergosterole in fungal cell membrane
- mammalian cells use cholesterol
Mode of action of antihelminthics
Ascaracides for worm infestation e.g. threadworm
- Paralyses worm by effect on nervous system
- not absorbed
Copyright eBook 2019, University of Leeds, Leeds Institute of Medical Education.