Pharmacokinetics – ADME
Examines the way in which the body handles drugs:
- Absorption of drugs into the body
- Distribution around the body
- Metabolism
- Elimination
This is an active process where all are occurring at the same time
Why is the study of pharmacokinetics important?
If a drug is going to have an effect in the body it needs to be present:
- In the right place
- At the right concentration
- For the right amount of time
Knowledge of pharmacokinetic data about a drug tells us:
- What dose to give
- How often to give it
- How to change the dose in certain medical conditions
- How some drug interactions occur
Absorption
Definition: The passage of a drug from its site of administration into the plasma
Three strategies for getting drugs into the system
- alter the physico-chemical properties of drugs
- change the formulation of drug
- administer by various routes
What are the factors affecting drug absorption?
- Compliance
- Food
- Enhance e.g. ketoconazole
- Impair e.g. tetracyclines, penicllin V, alendronic acid
- Formulation
- Enteric coated
- Slow or modified release (SR, MR)
- Route of administration
- IV = complete absorption (directly into blood stream)
- Oral = partial absorption
- Lack of specific carrier needed for absorption e.g. Intrinsic
Absorption and GI Motility
- Most drugs absorbed from the small intestine, not the stomach
- Gastric motility affects speed of onset
- Any delay is most important when first doses are being given
- Disease – (e.g. migraine + diabetic neuropathy)
| Site of drug absorption: | If drug absorbed from stomach, could bypass absorption site e.g. E.C preparations, PEJ tubes |
|---|---|
| Malabsorption syndromes: | e.g. Cystic Fibrosis |
| GI motility: | Rapid GI transit e.g. Crohn’s Disease, pro-kinetic drugs. |
| Inactivation of drug in gut or liver: |
e.g. insulin destroyed by proteolytic enzymes or first pass effect |
| Pre-existing medical Conditions: |
e.g. Acute Congestive Heart Failure |
| Drug interactions: | e.g. ciprofloxacin + calcium or iron, tetracyclines with milk, penicillin with food |
Distribution
Definition: The movement of a drug to and from the blood and various tissues of the body (for example, fat, muscle, and brain tissue) and the relative proportions of drug in the tissues
What are the factors affecting drug distribution?
- Plasma protein binding
- Competition for protein binding sites
- Specific drug receptor sites in tissues
- E.g. domperidone does not cause extra pyramidal side effects because it doesn’t reach dopamine receptors in the brain
- Regional blood flow
- Reduced blood flow
- Enhanced blood flow
- Lipid solubility
- Blood/brain barrier
- Membrane of GI tract e.g.. vancomycin
- Highly water soluble drugs e.g. gentamicin
- Disease
- Liver disease can cause low plasma protein levels
- Renal disease causes high blood urea levels
Protein Binding
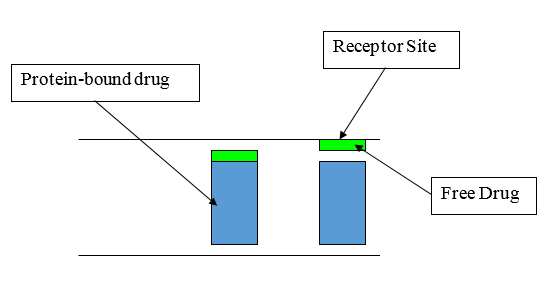
Plasma Protein Binding
- Many drugs bound to circulating plasma proteins such as albumin
- Only free drug can act at receptor site
| > 95% bound | > 90% but < 95% bound |
|---|---|
| Warfarin | Phenytoin |
| Furosemide | Sodium Valproate |
| Imipramine | Propranolol |
| Thyroxine | Glibenclamide |
| Diazepam | |
| Heparin | |
| Amitriptyline | |
| Diazepam |
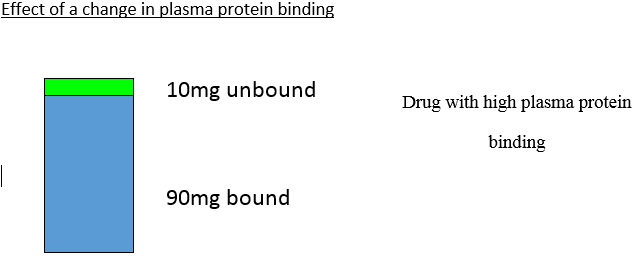
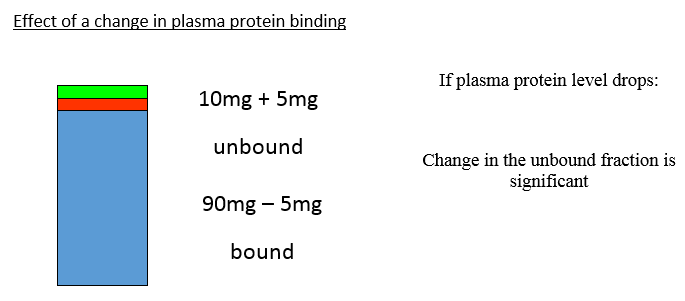
Changes in plasma protein binding are significant for drugs which are greater than 90% bound to plasma proteins
What are the factors which can increase the fraction of unbound drug?
- Renal impairment due to rise in blood urea
- Low plasma albumin levels (<20-25g/L)
- E.g. chronic liver disease, malnutrition
- Late pregnancy
- Decreased albumin production so fraction of unbound increased, but diluted by increased blood volume and it is the concentration that is important
- Displacement from binding site by other drugs
- e.g. aspirin, sodium valproate, sulphonamides
- Saturability of plasma protein binding within therapeutic range
- e.g. phenytoin
Copyright eBook 2019, University of Leeds, Leeds Institute of Medical Education.