Children have different fluid requirements to adults.
The normal osmolality for plasma is 270-300 mOsm/L. To prevent iatrogenic hyponatramia hypertonic intravenous fluids are used as standard in children (see table below).
Children requiring intravenous (IV) fluids should be administered fluids containing Glucose as children are at higher risk of hypoglycaemia and therefore the Glucose will meet some of their energy requirements.
Therefore for most hospitals the standard maintenance fluids for children will be either of:
• Sodium Chloride 0.9% and Glucose 5%
• Sodium Chloride 0.45% and Glucose 5%
Table: Types of fluids available |
||
Type of solution |
Name |
Ingredients in 1000mls |
Hypotonic |
Sodium Chloride 0.45% | 77 mEq Sodium, 77 mEq Chloride |
Isotonic |
Sodium Chloride 0.9% | 154 mEq Sodium, 154 mEq Chloride |
| Glucose 5% | 5 grams dextrose (200kcal) |
|
Hypertonic>300mOsm/L |
Glucose 10% | 10 grams dextrose (400kcal) |
| Glucose 5% with Sodium Chloride 0.45% | 5 grams Dextrose (200kcal), 77 mEq Sodium, 77 mEq Chloride |
|
| Glucose 5% in Sodium Chloride 0.9% | 5 grams Dextrose (200kcal), 154 mEq Sodium, 154 mEq Chloride |
|
| Lactated Ringer's | 130 mEq Sodium, 4 mEq Potassium, 3 mEq Calcium, 109 mEq Chloride, 28 mEq Sodium Lactate | |
However, there may be different fluid types used depending upon the underlying medical condition. For example, newborn and premature babies requiring IV fluids may be on 10% dextrose infusions, designer fluids or total parenteral nutrition (TPN). Typically 500ml bags of fluid are used in paediatrics.
All children on IV fluids should have a daily assessment of their electrolytes to identify and monitor any electrolyte imbalance. More frequent U&E monitoring may be required is there is a significant risk of or a known electrolyte imbalance.
It is also important to consider potassium when prescribing fluids. As a rough guide the electrolyte requirements for children are:
• Sodium 2-3mmol/kg/day
• Potassium 1-2mmol/kg/day
However, the overall amount of potassium required will depend upon any underlying electrolyte disturbance and medications (e.g. salbutamol and insulin drive potassium into cells). If potassium is required then it is standard to choose a fluid already containing 10mmol potassium chloride to a 500ml bag (i.e. 20mmol/l). However, 20mmol (i.e. 40 mmol/l) may need to be chosen in some circumstances. The quantity of potassium should be included on the prescription.
Daily maintenance fluids beyond the neonatal period are calculated depending on a child's weight and are prescribed in ml/hr.
Divide total by 24 to give rate in ml per hour |
In adult practice a bag of standard intravenous fluid may be administered by hanging the bag from a drip stand and titrating the rate by "drip rate" (i.e. the number of drips seen per second). In paediatrics this would not be safe. Fluids are always given through an electronic fluid pump at a set hourly rate with a set total volume of fluid to be administered. This is to ensure that the correct rate is given but more importantly that an excess volume of fluid is not given. During resuscitation a bolus of fluid may be given manually with a 50ml syringe (for intravenous) or 20mls syringe (for intraossesous).
Katie Clough is 2 months of age and has been admitted with bronchiolitis. She weighs 5kg. She is unable to tolerate enteral feeds (NG or oral) and therefore needs intravenous maintenance fluids. Please calculate her maintenance fluids
5kg x 100ml = 500ml
Total = 500ml/24hours
= 21 mls/hr
James is a 3 year-old weighing 14kg. Please calculate his maintenance fluids
10kg x 100ml = 1000ml
4 kg x 50ml = 200ml
Total = 1200ml/24hours
= 50 ml/hr
Beatrice is an 8 year-old weighing 28 kg. Please calculate her maintenance fluids.
10kg x 100ml = 1000ml
10kg x 50ml = 500ml
8kg x 20ml = 160ml
Total = 1660ml/24 hours
= 69ml/hr
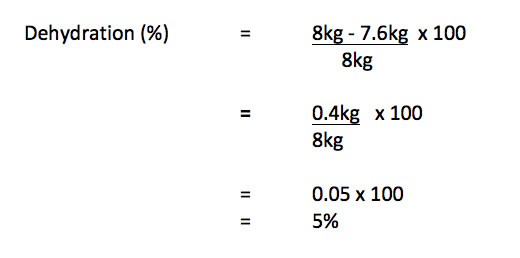
Some children presenting to or admitted to hospital will be dehydrated. It is important to assess the degree of dehydration to calculate overall fluid requirements. Percentage dehydration can be calculated either using weight, if a recent weight is known or based on clinical assessment.

An 8kg infant with diarrheoa and vomiting now weighs 7.6
Most times there is not a recent reliable weight available and therefore the level of dehydration needs to be calculated using clinical parameters. This is an estimation of the degree of dehydration.
"More numerous and more pronounced symptoms and signs of clinical dehydration indicate greater severity. For clinical shock, one or more of the symptoms and/or signs listed would be present. Dashes (–) indicate that these clinical features do not specifically indicate shock. Symptoms and signs with red flags may help to identify children at increased risk of progression to shock. If in doubt, manage as if there are symptoms and/or signs with red flags. " (NICE CG84)
• Clinical signs of dehydration are only detectable when the patient is 2.5-5% dehydrated.
• As a guide, the child with dehydration and no shock can be assumed to be 5% dehydrated.
• If shock has occurred then usually ≥ 8-10% dehydration has occurred.
• Sometimes the maximum percentage dehydration clinicians will use is 8% to avoid overestimation of fluid requirements.

This is then given with maintenance fluids over 24 hours.
For example a child (Ghanta Sam) who weighs 15kg who is 5% dehydrated
Fluid deficit (ml) = 5% dehydration x 15kg x 10
= 750ml (over 24 hours)
= 31mls/hr
Total fluid requirement = maintenance fluids (ml) + fluid deficit (ml)
Daily maintenance fluids = (10kg x 100) + (5kg x 50ml)
= 1250 ml
Total fluid requirement (for first 24 hours)
= 750mls + 1250mls
= 2000mls
= 83.3mls/hr
This would usually be given as a standard intravenous fluid (e.g. 0.9% saline with 5% dextrose +/- potassium)
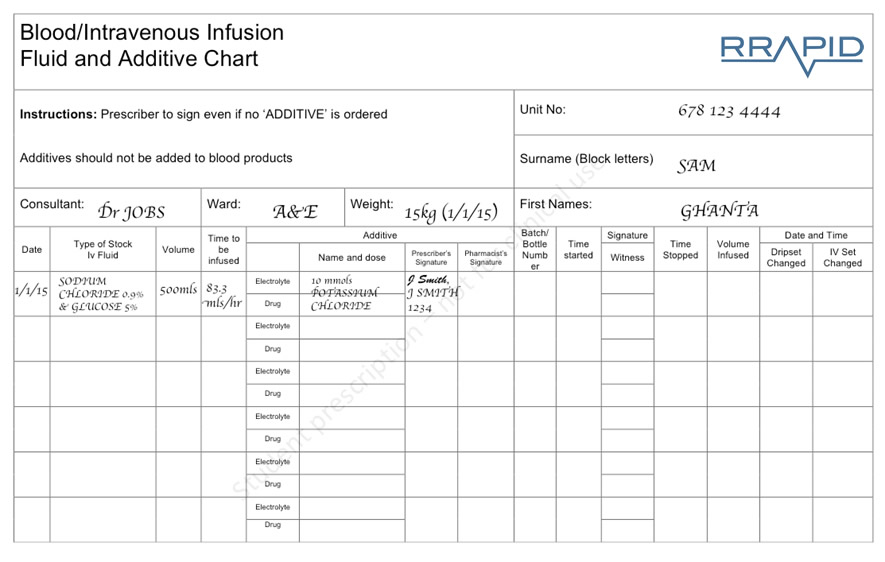
View larger image
This should therefore correct the fluid deficit over 24hours. This therapy should be monitored every 3–4-hourly intervals using weight as an objective measure. This is to ensure that the patient is gaining weight at an appropriate rate.
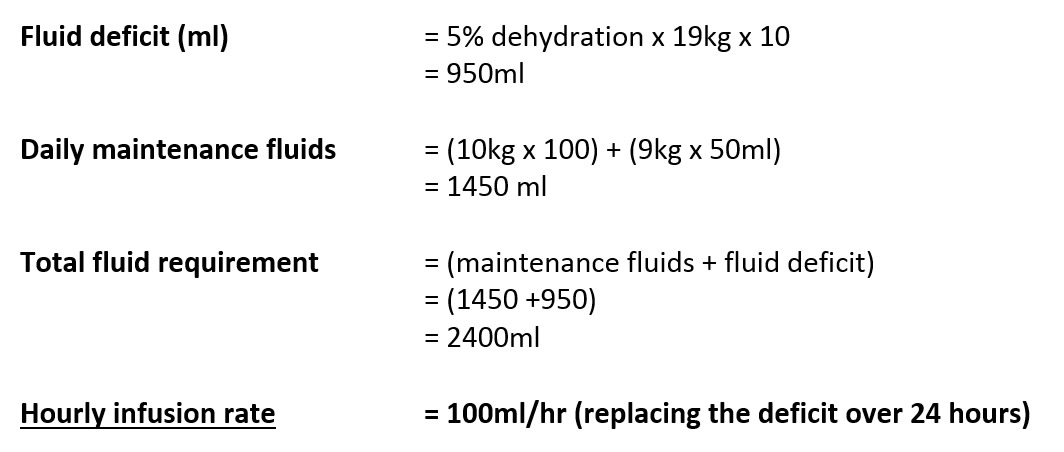
Ella is a 5 year-old girl admitted with gastroenteritis for the past 24 hours. She is not shocked. She is unable to tolerate enteral fluids and needs intravenous fluids. Clinically she is 5% dehydrated. Please calculate her fluid requirement for 24 hours and the hourly infusion rate. She weighs 19kg.
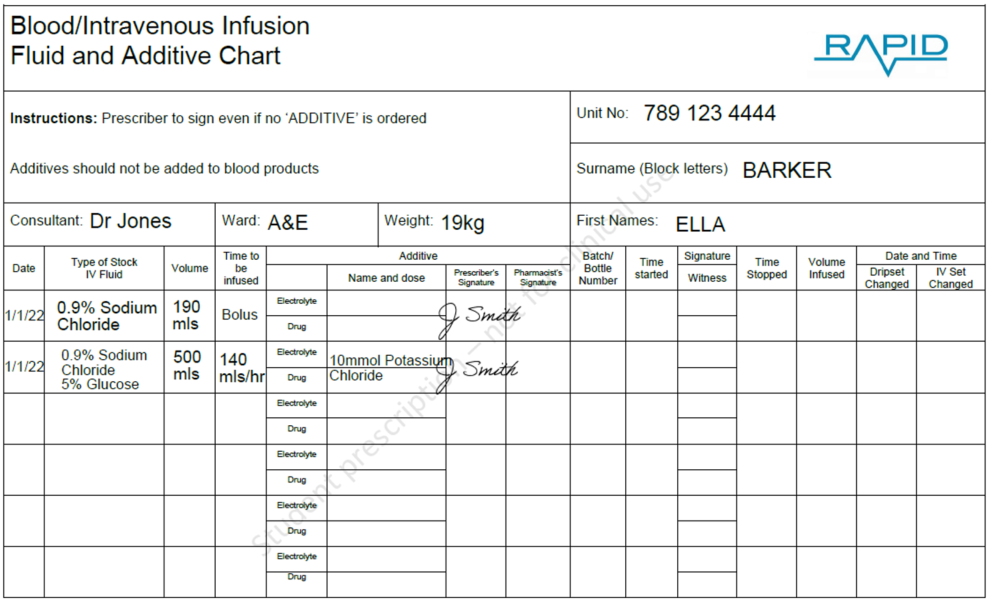
Ella Barker is a 5 year-old girl admitted with gastroenteritis for the past 24 hours. She is shocked. Clinically she is 10% dehydrated. Please calculate the first fluids that you would like the nursing staff to administer. Ella weighs 19kg.
Bolus = weight (kg) x 10mls
= 19 x 10
= 190mls (given as normal saline 0.9%)
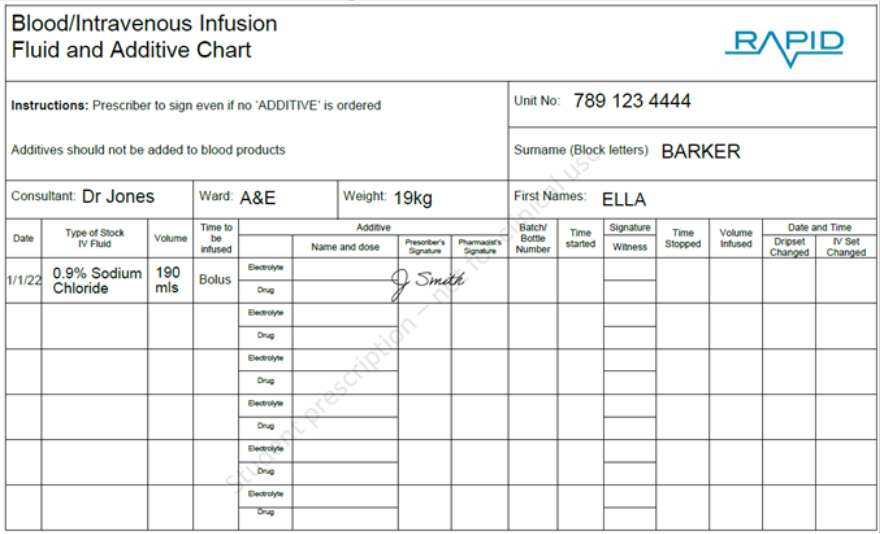
View larger image
You will notice that a "bolus" has been prescribed. This can be prescribed as "bolus", "stat" or "5 minutes" etc. The key is that the correct volume is prescribed and that it is given rapidly (i.e. under 10 minutes).
Also, there is a "line-through" the additive section if you do not wish an additive (such as potassium) to be added.
Maintenance fluids once a bolus is given
There is no one correct answer about how to give maintenance fluids once a bolus has been given, however a simplified approach is likely to minimize errors.
In the APLS course (ALSG) it is recommend that "once shock has been adequately treated, attention can turn to management of hydration". Management of dehydration consists of administration of calculated daily maintenance fluids in addition to calculated deficit. The APLS course does not recommend removing the bolus from this calculated deficit. This is supported by the NICE guidance on intravenous fluids in children.
Therefore even when a bolus has been given the equation for fluids for first 24 hours remains the same:
Total fluid requirement = Maintenance fluid + fluid deficit
Ella Barker is a 5 year-old girl admitted with gastroenteritis for the past 24 hours. She is shocked and you have prescribed her fluid bolus. Clinically she is 10% dehydrated. Please calculate her fluid requirement for 24 hours and correctly prescribe her first bag of maintenance fluids. She weighs 19kg.
Fluid deficit (ml) = 10% dehydration x 19kg x 10
= 1900ml
Daily maintenance fluids = (10kg x 100) + (9kg x 50ml)
= 1450 ml
Total fluid requirement = (maintenance fluids + fluid deficit)
= (1450 + 1900)
= 3350ml
Hourly infusion rate = 139.6ml/hr (replacing over 24 hours)
Some clinicians will take the bolus volume off the deficit (i.e. Total fluid requirement = Maintenance fluid + (fluid deficit - boluses). This is not "incorrect" it is just not the method imployed by APLS or NICE.
View larger image
You will notice that a bolus has been prescribed already. A 500ml bag will run out after approximately 4 hours. If there is shock and 10% dehydration the patient should have a fluid review after 4 hours (ideally with a weight). By this point a U&E should hopefully be available.
Also, there is a "line-through" the additive section if you do not wish an additive (such as potassium) to be added. There is no absolute correct answer to when or how much potassium to add.
There is more information on fluid prescribing in children at the NICE website
(https://www.nice.org.uk/guidance/ng29/chapter/Recommendations#principles-and-protocols-for-intravenous-fluid-therapy )
In this case the child was unable to take enteral fluids. If the gut is functioning, oral (or nasogastric) the child can be rehydrated using standard Oral Rehydration Solutions (ORS). The WHO ORS formulation provides 75 mmol Na, 20 mmol K, 65 mmol Cl, 10 mmol citrate and 75 mmol glucose per litre. The ORS formulations generally used in the UK have a lower Na concentration (50–60 mmol/l).
Note: the glucose contained in ORS is to aid absorption of the fluid through the gut wall and will not maintain or improve a blood sugar level
ORS should be administered frequently in small volumes (e.g. a cup and spoon). Generally normal feeds should be administered in addition to the rehydration fluid, particularly if the infant is breast-fed.
It is possible to use the same calculation as above to calculate the maintenance and deficit. As the enteral route is being used the deficit can be given quicker with the UKs NICE recommending that in children with dehydration 50mls/kg of ORS can be given over 4 hours.
Ella is a 5 year-old girl admitted with gastroenteritis for the past 24 hours. She is not shocked. She is able to tolerate enteral fluids and needs enteral fluids. Clinically she is 5% dehydrated.
Please calculate her maintenance fluid requirement for 24 hours and the hourly rate. She weighs 19kg.
Daily maintenance fluids = (10kg x 100) + (9kg x 50ml)
= 1450 ml
= 60mls/hour (over 24hours)
What volume of fluid would she require to replace her 5% dehydration? She weighs 19kg.
Fluid deficit (ml) = 5% dehydration x 19kg x 10
= 950ml
This fluid deficit is often replaced enterally over four hours rather than 24 hours. Therefore what would her hourly rates?
Daily maintenance fluids = (10kg x 100) + (9kg x 50ml)
= 1450 ml
= 60mls/hour (over 24hours)
Fluid deficit (ml) = 5% dehydration x 19kg x 10
= 950ml
= 240mls/hr (over four hours)
Total fluid requirement = 300mls/hour for four hours followed by 60mls/hour