0 – 12 months: Weight (in kg) = (0.5 x age in months) + 4 1 – 5 years: Weight (in kg) = (2 x age in years) + 8 6 – 12 years: Weight (in kg) = (3 x age in years) + 7 |
Q – Kamal is a 3 year old boy who was found face down in a pond. You need to give adrenaline. What is his predicted weight?
14kg
Q – Sarah is a 11 year old girl with suspected septicaemia. You need to give intravenous antibiotics and fluids. What is her predicted weight?
40kg
Q – Jack is a 3 month old boy who has been found lifeless at home. You need to give adrenaline. What is his predicted weight?
5.5kg
Q – Aaron is a 2 year old boy who has croup. You need to give oral dexamethasone. What is his predicted weight?
12kg
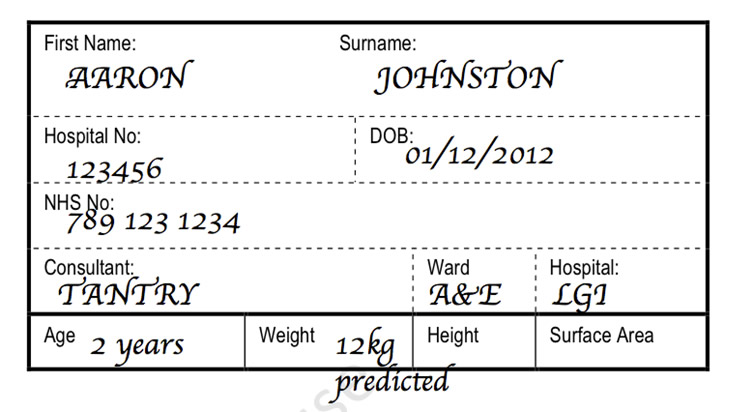
You will notice that on this prescription for Aaron that the 12kg weight has been clearly marked as "predicted". This is to ensure that those writing prescriptions know that the weight is predicted and that as soon as the child is well enough that the child should be formally weighed.
Whenever weight estimations are being used, it is important to get an actual weight at the safest opportunity. |
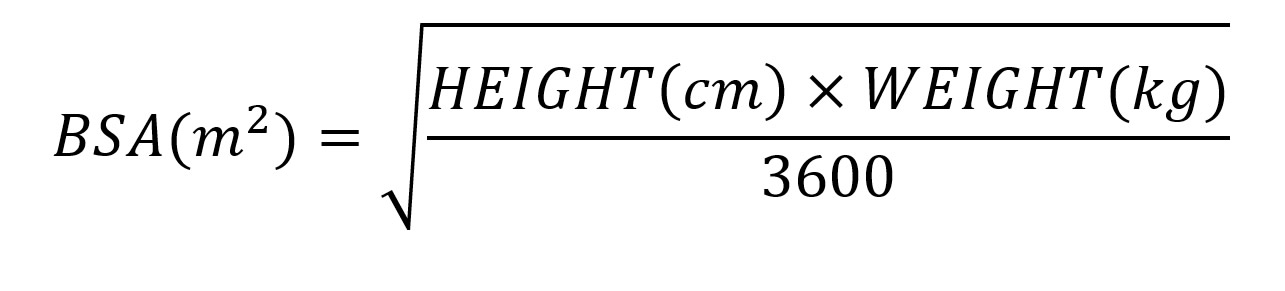
Occasionally, some doses of medication are standardised by body surface area (BSA). This is because many physiological phenomena correlate better with body surface area then with weight. One of the most common medicines prescribed using surface area in an acutely unwell child is intravenous Aciclovir.
There are charts available (e.g. in the rear of the BNFc) which can convert weight into an appropriate surface area. These are more commonly used as they are less likely to lead to calculation errors (see equation below) and also do not require a child's height to be taken.
At times the surface area is calculated. To calculate body suface area the most commonly used equation is the Mosteller method
Each hospital will have it's own drug chart. These are often paediatric specific. These will include all the necessary spaces to ensure the correct information is given to the nurses and/or doctors administering the medications. They will usually include three sections:
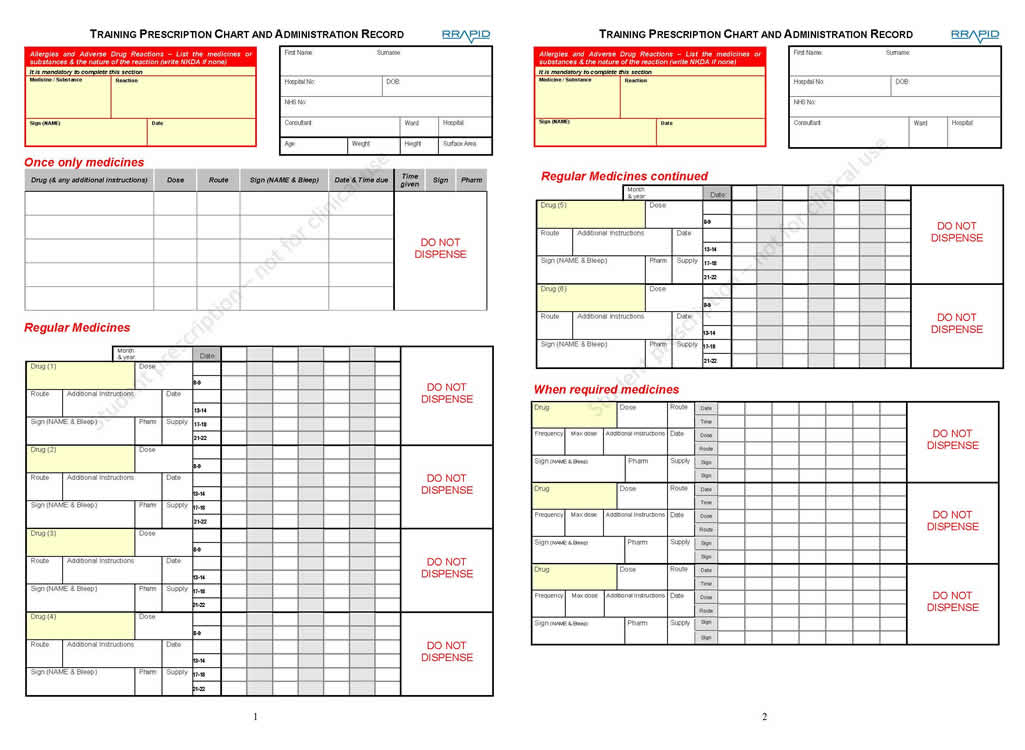
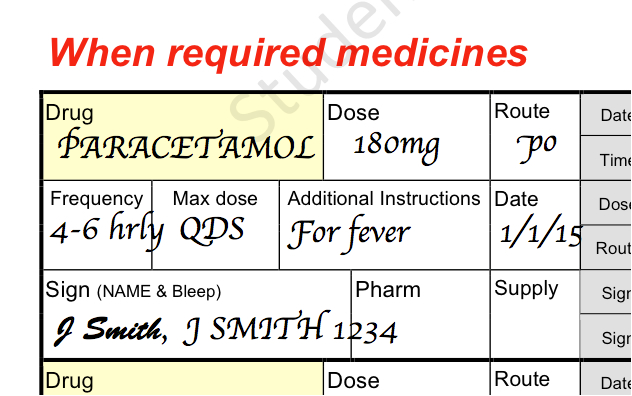
Gemma is a 3 year 11 month old girl who has fever secondary to UTI which is causing abdominal pain. She is being admitted and you have been asked to prescribe paracetamol.
How much paracetamol would you prescribe, how often and where on a drug chart.
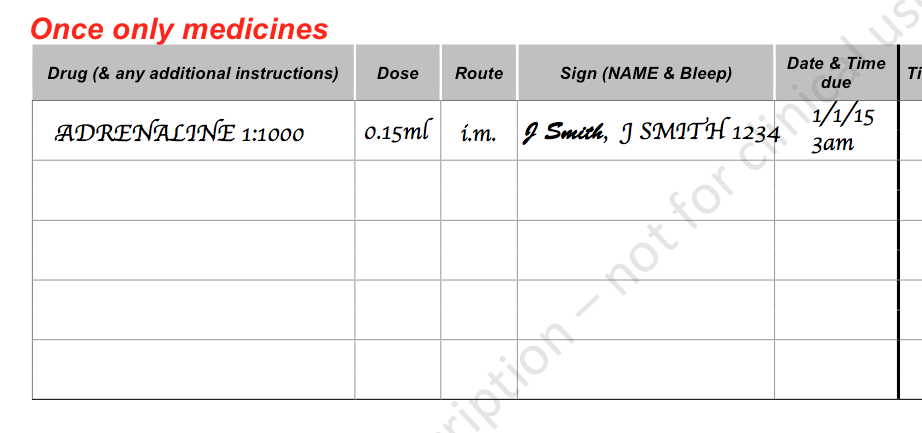
Avanish is a 5 year old boy who presents with anaphylaxis having eaten a collection of snacks at a birthday party.
How much adrenaline would you prescribe, how would you give it, how often and where on a drug chart.
It is 8pm. Ester is 2 years of age and has suspected septicaemia. Predicted weight is 12kg. You have inserted a cannula and sent blood cultures. You want to start antibiotics and therefore want to prescribe ceftriaxone.
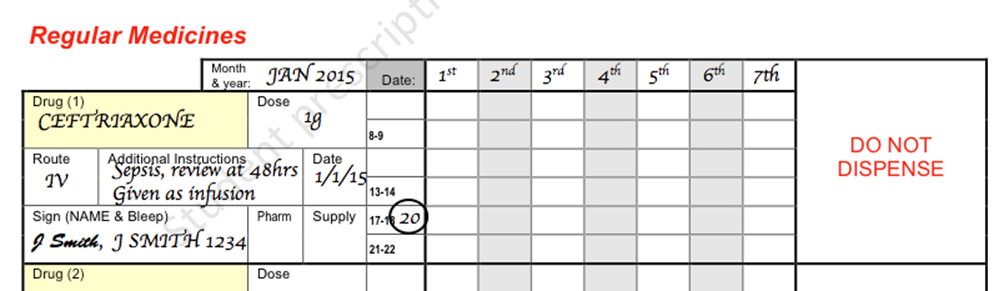
In this case a dose of 960mg is a correct dose and would be a correct prescription. In this case a prescription of 1g has been written. Note that the month, year and dates have been put in the banner above the prescription.
At times a medication may need to be given at a regular time each day but you want to demonstrate to the person administrator of the medication (e.g. the nurse) that you want this medication to stop on a particular day.
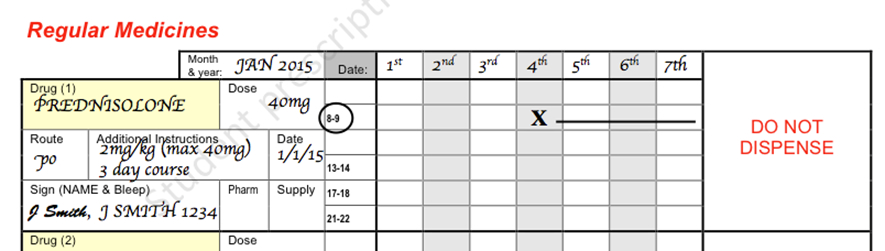
An example of this would be prednisolone which is usually given for 3 days in acute exacerbation of asthma. In this chart you will see that the prescriber has left space for medication to be given for three days. This has been done with a cross and line so that that the drug cannot be given on those days at that particular time.