Video: The Full Paediatric BLS sequence (also available at https://youtu.be/V_6DTzS--3M)
Safety: Approach with care, ensuring you are free from danger. A rescuer should never put themselves in danger, as this risks creating a second victim. If the environment is dangerous the child should be removed from danger as quickly as possible. This safety is paramount and precedes an airway assessment.
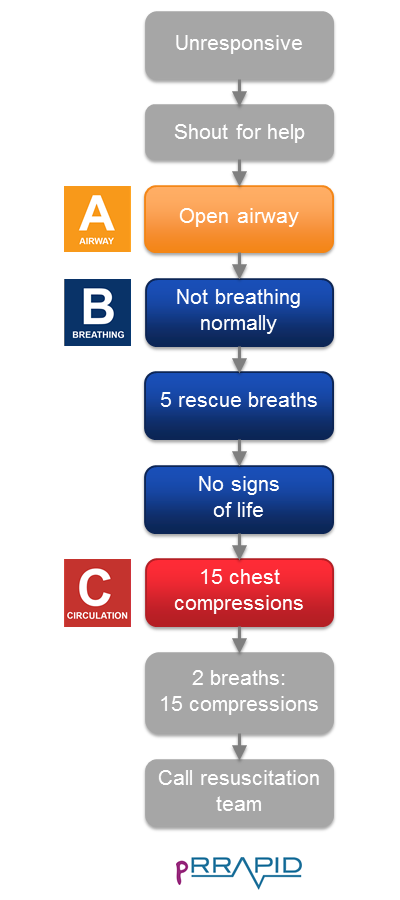
Stimulate: Gently apply stimulus and ask “Are you alright?” A recommended stimulus would be to hold the head and shake the arm. You are making an immediate assessment of their responsiveness. Be aware that infants and children may not respond meaningfully.
Shout: For health care professionals most cases of resuscitation will occur in a healthcare facility. Shouting for help could include: pulling an emergency alarm, shouting or sending another staff member or carer to raise the alarm. Resuscitating a child often requires a large team. Roles and responsibilities are delegated within this team, therefore it is good practice to call a “paediatric resuscitation team” early. Whilst waiting for help to arrive the rescuer should progress with sole-rescuer BLS.
Special considerations: When there is a lone rescuer and assistance has not arrived after 1 minute of CPR then the rescuer must activate the Emergency Medical Services (EMS) system themselves. If CPR is being performed on a baby or small child then the rescuer is likely able to carry the victim with him or her to a telephone whilst attempting to continue CPR on the way. Thankfully with easy access to mobile telephone technology, with speaker phones, these eventualities are now much less common and help can be called whilst providing assistance.