The causes of tachy-arrhythmias in children include:
The causes of brady-arrhythmias in children include:
Presentation can include


Table: Normal vital signs in children |
|||||
Infant |
1-2 years |
2-5 years |
5-12 years |
Adolescent |
|
Pulse rate (bmp) |
110-160 |
100-150 |
95-140 |
80-120 |
60-90 |
Respiratory rate (rpm) |
30-40 |
25-35 |
25-30 |
2-25 |
14-18 |
Blood pressure Systolic mmHg |
80-90 |
85-95 |
85-100 |
90-100 |
100-140 |
Temperature (define if oral etc) |
35-37oC |
36-37.5 oC |
|||
Saturations |
94-98% |
||||
A thready pulse, with hypotension and delayed capillary refill suggests haemodynamic instability.


All cardiac arrhythmias, particularly if unstable, require the same initial response:


The treatment options will depend on the above and the child's stability


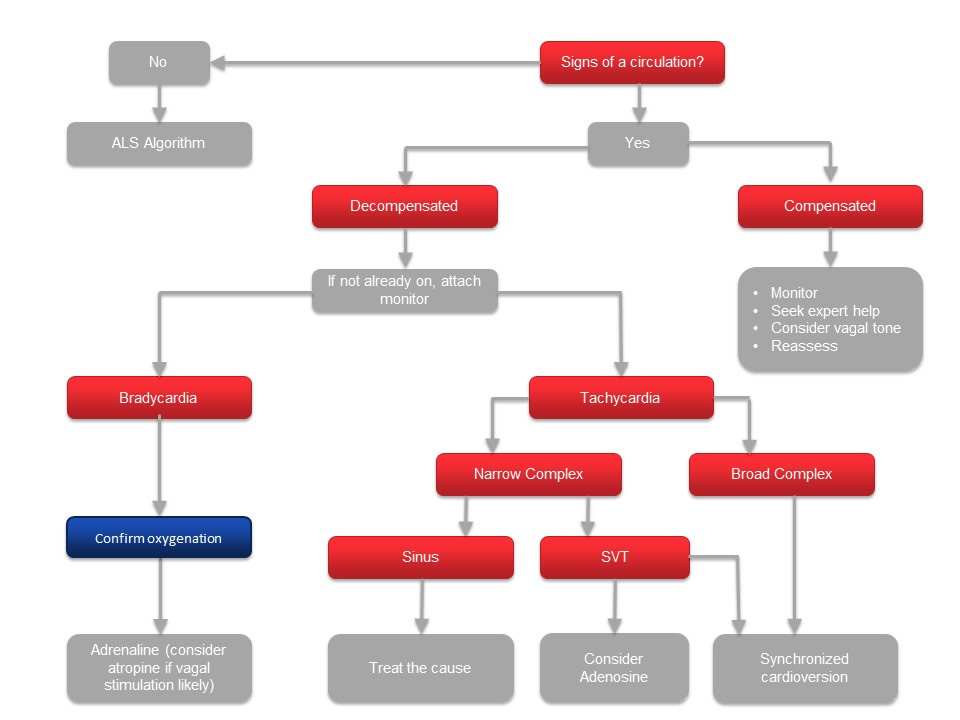
Essentially, there are a series of questions you need to ask yourself when you see a child with a cardiac arrhythmia
Question 1- Is there a central pulse and signs of life?
Yes - Continue to Question 2.
No - You will need to treat this as cardiopulmonary arrest and start the
Advanced Paediatric Life Support Algorithm
Question 2 - Is the patient haemodynamically stable?
Yes -
• Monitor the patient closely
• Since they are stable you have time to seek expert help.
• Contact an expert as soon as possible
• Move onto question 3
No -
• Call for urgent help
• Move onto question 3 as you need to identify the type of arrhythmia it is in order to treat it appropriately.
Question 3 - What is the heart rate? Is it fast or slow?
This will help you identify the cause of the arrhythmia and narrows down your treatment options.
Bradycardia
• Caused commonly by hypoxia, acidosis or severe hypotension. It can quickly progress to cardiopulmonary arrest.
• Ensure the patient is well oxygenated and ventilated
• If a poorly perfused child has a heart rate of less that 60 beats per minute and they do not respond to ventilation and oxygen – start chest compressions with the use of adrenaline and treat as cardiopulmonary arrest as per the Advanced Paediatric Life Support algorithm.
• If the bradycardia is thought to be due to shock – treat with 0.9% saline (20mg/kg bolus). Consider using adrenaline if this is ineffective
• If the bradycardia is caused by vagal stimulation (eg. following passing an NG tube), atropine may be helpful in correcting this
• Cardiac pacing is not useful during resuscitation but may be used when the patient is haemodynamically stable. You would need to seek expert paediatric cardiology input for this.
Tachycardia
If the heart rate is fast you need to ask yourself one further question – Go to question 4
If the heart rate is fast you need to ask yourself the following question:
Question 4 - Is the QRS complex narrow or broad?
Sinus tachycardia has a number of causes. The treatment needs to be tailored to the cause. For example, a 20mg/kg bolus of 0.9% normal saline would be a sensible first line management if hypovolaemia was thought to be the cause. IV antibiotics would be needed if sepsis were suspected.

If SVT is the likely rhythm (very fast heart rate, no p waves seen):
In a haemodynamically stable patient:
In a haemodynamically unstable patient:
Click below for the algorithm which explains the management very clearly
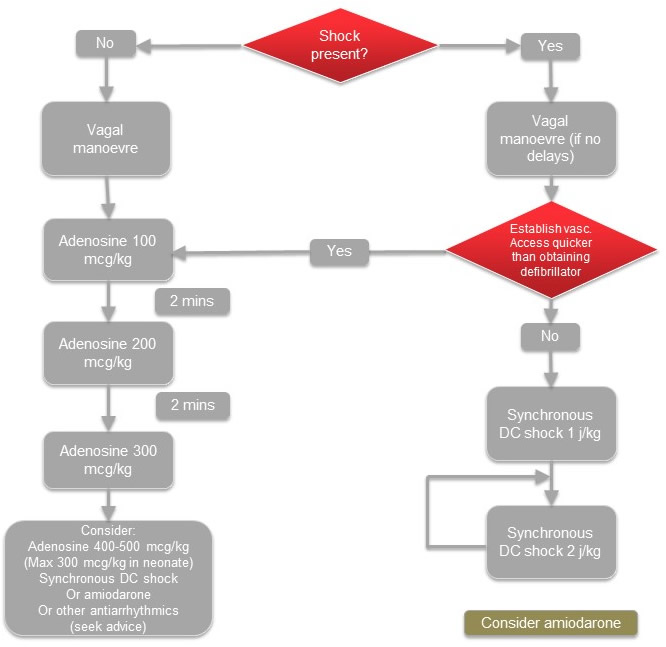
Figure: SVT management
Broad complex tachycardias are considered to be ventricular tachycardias until proven otherwise. They are uncommon in children, mostly occurring in those with underlying heart problems. It is imperative that blood electrolytes (U&E, Calcium and Magnesium) are checked, as electrolyte disturbances are also a cause.
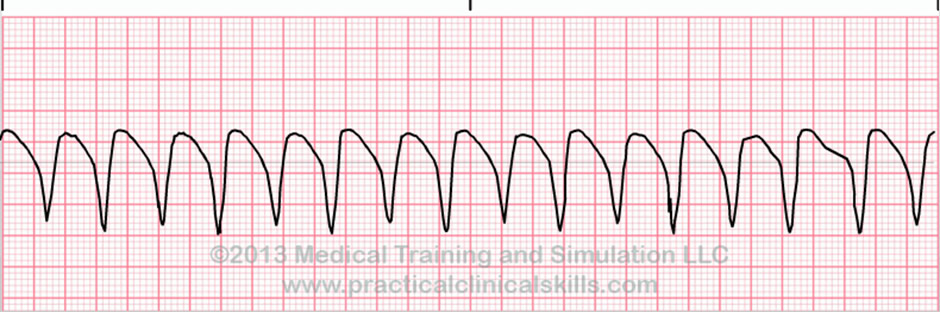
Give a synchronised DC Shock (1J/kg), and repeat if needed (2J/kg). Consider amiodarone if no improvement.
Early consultation with a paediatric cardiologist would be advised. They may suggest using IV amiodarone or IV procainamide.
There are many different types of arrhythmias which are beyond the scope of this course but if you are able to answer the key 4 questions we have discussed, you will be able to start some life saving interventions before your help arrives:
So remember to ask yourself:
The diagram on the below helps to summarise these points.