Being able to describe rashes and link these to common conditions/emergencies is important (see table)
Table: Skin lesions/rashes |
|||||
Example |
Description |
Causes |
|||
| Petechiae Micro-haemorrhage appearing as 1-2mm red, purple or brown macule |
Septicaemia Bleeding disorder (including ITP) |
||||
| Purpura Bleeding into the skin (often multiple petechiae). Purpura do not blanch with pressure |
|||||
| Ecchymosis A common bruise (a form of purpura) |
Infection (purpura – see above) Trauma Bleeding disorder |
||||
| Macular <5mm, blanching, non-palpable lesion |
Viral infection:
Drug reactions Early septicaemia |
||||
| Papular <5mm, blanching, palpable lesion |
|||||
 |
Vesicular <5mm fluid filled, circumscribed, epidermal lesion |
Varicella (chickenpox) Shingles Herpes simplex Coxackie (hand, foot and mouth) |
|||
 |
Bullous/Pustular >5mm fluid filled, circumscribed, epidermal lesion. Contain clear or purulent fluid respectively |
Impetigo Scalded skin syndrome |
|||
 |
Erythema Redness caused by vascular dilatation |
Viral exanthema Burns Scalds Injuries |
|||
 |
Wheal (urticarial) | Allergy Anaphylaxis Idiopathic |
|||
 |
Angioedema | ||||
Images copyright DermNet NZ, reprinted with permission. |
|||||
A core temperature should always be taken. In children the temperature should be taken using one of the following methods:

Fever: Fever suggests an infective cause for the severely unwell child. The causes of fever are extensive. Common paediatric
Table: Causes of fever (not comprehensive) |
|||||
Infection |
Viral |
Upper respiratory tract infection (e.g. pharyngitis, acute otitis media, croup etc) |
|||
Bacterial |
Pneumonia |
||||
Fungal |
|||||
Parasites |
Malaria |
||||
Collagen vascular disorders |
Juvenile idiopathic arthritis |
||||
Malignancies |
Hodgkin disease |
||||
Miscellaneous |
Kawasaki disease |
||||
Hypothermia: Young children with infection may present with hypothermia rather than fever. Hypothermia can also be caused by inadequate clothing/exposure.
History taking is covered in the paediatric history chapter of this resource
The child must be appropriately exposed to complete your examination, however, it is important to respect dignity at all times and minimise heat loss. Once you have performed your initial assessment (and responded appropriately (primary survey) it would be appropriate to perform another more thorough examination as part of the secondary survey. This is generally a top to bottom examination focusing into any systems examination where relevant.
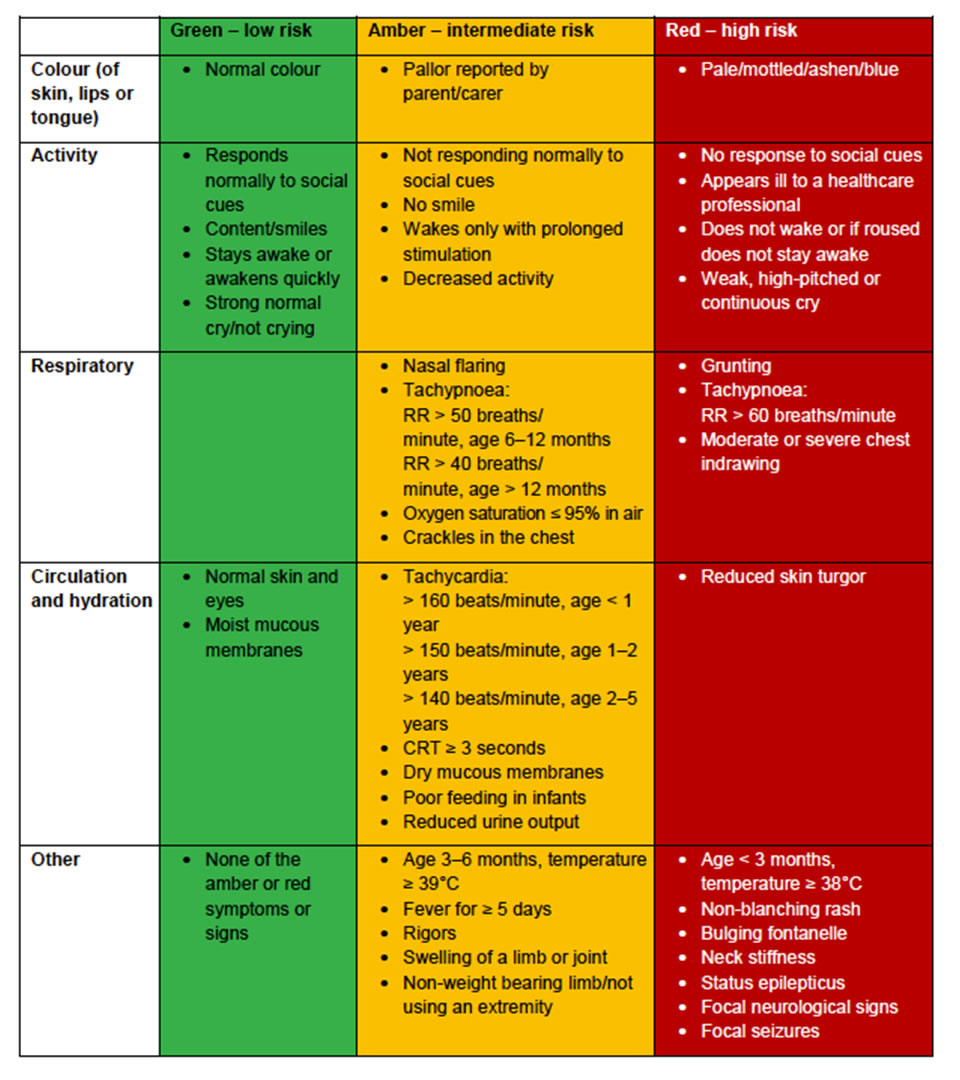
This will include an examination of the major systems and identifying features such as those described in this table.