It is 2am. You are a junior doctor on night shift. You are bleeped by one of the members of the nursing team on the paediatric ward.
S
Hi, it's Helen here. I'm the nurse looking after Eddie Mico on the paediatric ward. Is that the junior doctor?
I'd like you to come review one of the patient's on the ward immediately please.
B
Eddie Mico is a 2-year-old boy who has been admitted for observations overnight following a first febrile convulsion.
On admission a provisional diagnosis of viral upper respiratory tract infection was made. He's been febrile and had a convulsion at home.
He's normally fit and well
A
Since he was admitted he has deteriorated. He is maintaining his own airway and has normal respiratory rate and oxygen saturations. However, he is tachycardic with a heart rate of 164bpm and his hands and feet feel very cold. His temperature is 40 degrees Celsius and the fever doesn't seem to come down with paracetamol.
R
Can you come review him please? Is there anything you'd like me to do whilst you are on your way here?
Q – What would you like the nurse to do (RESPONSE) whilst you are on route to see the patient?
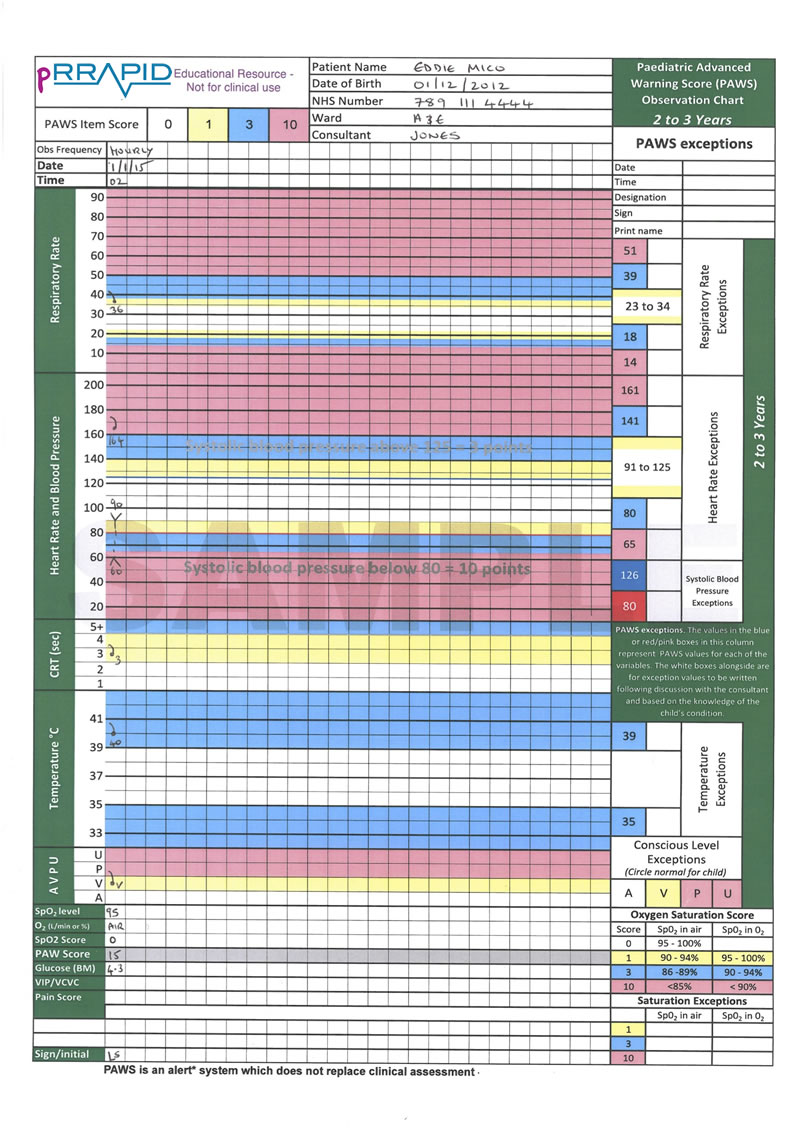
You have the following Paediatric Early Warning Score available from the observations that you asked the nurse to perform

As you approach you notice that Eddie is lying in bed, and not speaking.
Q – Recognition: How will you assess if the airway is patent
You assess airway patency by
• looking for chest and/or abdominal movement,
• listening for breath sounds and
• feeling for expired air.
You are reassured to note that you can see his chest moving, you can hear breath sounds and feel the expired air.
Q – Respond: how do you respond?
Eddie’s airway is patent and does not require an adjunct at this point. There are no signs of airway obstruction and you therefore move on to breathing.
Q – Recognition: How will you assess his breathing?
The nurse informs you that his saturations are 100% on the 15L of oxygen you requested. She tells you his saturations were 95% in room air previously. He is mildly tachypnoeic with a respiratory rate of 36rpm. His trachea is central and he has no chest recessions. His air entry is good and equal on both sides with no added sounds.
Q – Respond: how do you respond?

Q – Recognition: How will you assess his circulation?
He is tachycardic with a heart rate of 160bpm. The pulse volume is adequate. His blood pressure is 90mmHg systolic. His peripheries are cool. He has a central CRT of 3 seconds and a peripheral CRT of 4 seconds. He looks pale. His mother reports that he is very sleepy and hasn’t passed urine since he arrived on the ward 5 hours ago.
Q – Respond: how do you respond?
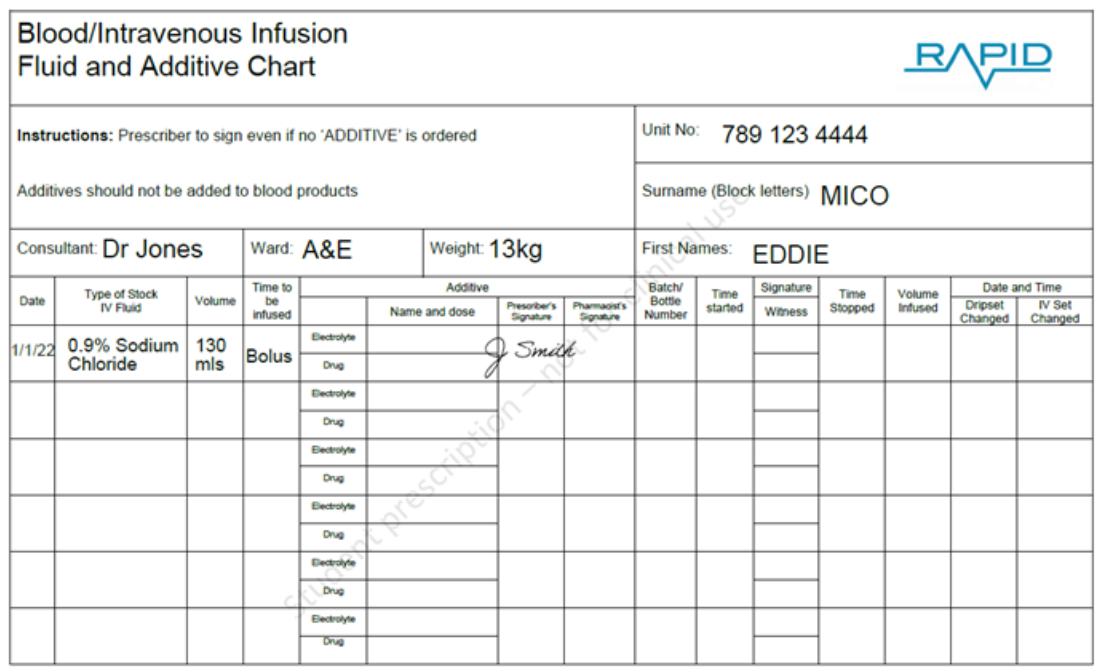
Q – Respond. Eddie’s admission weight was 13kg. Use the fluid chart in your pRRAPID pack to prescribe a fluid bolus for this patient.
Eddie Mico
2 years old.
Hospital number 123444
NHS no. 789 111 4444
NKDA
Weight 13kg
Consultant: Dr Tantry
Bolus = weight (kg) x 10mls
= 13 x 10
= 130mls (given as Sodium Chloride 0.9%)

Q – Recognition: How will you assess disability?
You perform an AVPU assessment and find that he is responsive to your voice. His pupils are equal and reactive. His posture is normal. His capillary blood glucose is 4.3mmol/l. There is no seizure activity
Q – Respond: how do you respond?
You note that he may be slightly more drowsy that normal. You are satisfied with the remainder of his disability assessment at present, so you move onto exposure.
You note to yourself that you will reassess this, especially when the fever has resolved.

Q – Recognition: How will you assess “exposure”?
You expose Eddie and find and notice a rash.
pRRAPID: non-blanching rash video.
This video is also available at https://youtu.be/Qr9yK-MapO8
The rash is spreading from his toes up towards his knees. His temperature is 40.1o Celsius.
Q – Recognition: what do you think is the most likely differential diagnosis?
Meningococcal septicaemia with possible meningococcal meningitis. The child is shocked and so septicaemia needs to top of your differential list. The purpuric rash which you have identified on Exposure would certainly support this diagnosis.
The high fever and extreme tachycardia are a warning sign that this child could be a lot sicker then other findings may suggest. This is because the compensatory physiological responses are good in children.
It is entirely possible that he also has meningitis, especially considering his seizure, however it is possible he has septicaemia alone, especially as he is not “meningitic”. You would not be able to perform a lumbar puncture at this point as he is not cardiovascularly stable and he has a rash suggesting system meningococcal disease (see Disability chapter for contradictions for LP).
Q – Respond: how do you respond?
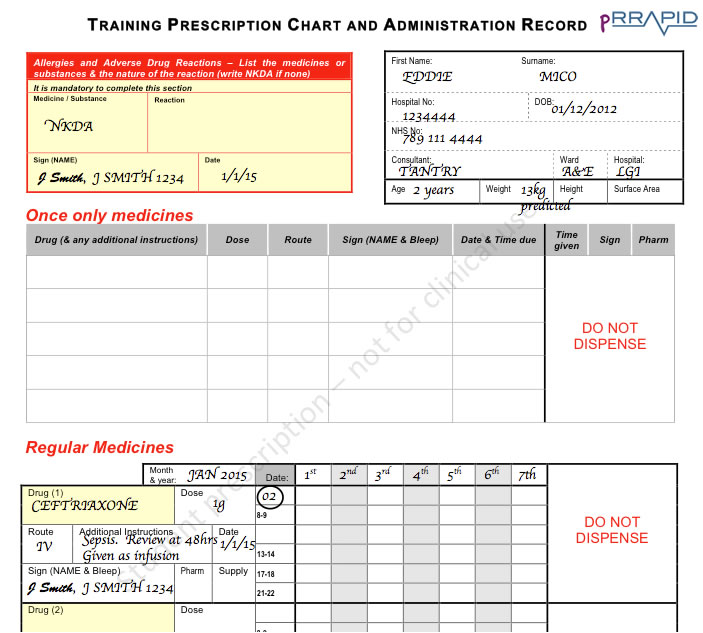
You are concerned that this non-blanching rash and fever with cardiovascular compromise is meningococcal septicaemia. You therefore want to prescribe and administer a dose of Intravenous Ceftriaxone.
Q – Use your pRRAPID prescription pack and write a drug chart for Eddie and prescribe intravenous ceftriaxone.
As this child has septicaemia he requires intravenous (IV) antibiotics. As it is a serious infection a prescription of 80mg/kg would be required. This should be therefore given as an infusion.
Dose = 13kg x 80
=1040mg
This is therefore rounded to a sensible dosing regimen of 1g daily.
History of presenting complaint: You take a history from his mother who tells you he has had a fever today and has been generally unwell with a “snotty nose”. He is otherwise normally fit and well and his immunisations are up to date. He has not been in contact with anyone who has been unwell.
Q –– Respond: pRRAPID pack to prescribe “as required” paracetamol.
Q – Respond: You contact your senior to inform them of the patient’s condition using an SBAR structure.
S
Hello, it’s Toby here the junior doctor on for the night shift. Is that the paediatric registrar speaking?
I’ve just reviewed Eddie Mico a 2-year-old boy who has deteriorated on the paediatric ward.
B
Eddie is normally a fit and well child who was admitted for observation following at febrile convulsion earlier today. The fever was initially felt to be secondary to a viral upper respiratory tract infection. The nurse asked me to review him because his temperature was persistently elevated and he was more tachycardic.
A
I’ve assessed him. He’s maintaining his own airway and is breathing independently and his chest is clear. He has a pulse rate of 160bpm associated with a CRT of 3 seconds and cold peripheries. His blood pressure is normal. He is responsive to Voice on the AVPU scale and his blood glucose is normal. He is febrile with a temperature of 40.1O Celsius and he has a spreading non-blanching purpuric rash to his legs. My primary concern is that he is shocked and that he has meningococcal septicaemia.
R
I have inserted a cannula and taken bloods including blood cultures and a venous blood gas. I’ve prescribed a 10mg/kg bolus of 0.9% saline, which is just being given. I’ll review the response to the bolus of fluid. We are going to monitor his fluid input/output.
I have prescribed IV Ceftriaxone at 80mg/kg and that is going to be given immediately after the bolus of saline.
I’ve not performed an LP as he has had a recent seizure and also he is cardiovascularly compromised with suspected meningococcal disease. I’d be very grateful if you could review the patient with me. As I mentioned, I’m going to review him now to assess if he needs another bolus.
His cardiovascular status has improved, his CRT is now 2s centrally and his heart rate has come down.
Q: Your senior doctor has asked you to prescribe maintenance fluids for Eddie. What fluid do you prescribe and how much?
10kg x 100ml = 1000ml
3kg x 50ml = 150ml
Total = 1150ml/24hours
= 48 ml/hr
You prescribe a hypertonic standard maintenance fluid such as 0.9% Saline & 5% dextrose OR 0.45% Saline & 5% Dextrose
Children’s potassium requirements are usually 1-2mmol/Kg/Day. Therefore if prescribing fluids for a 24 hour period this should be borne in mind. In this case the weight is 13kg therefore 10mmol/l in each bag would meet this requirement. Electrolytes should be checked at least every 24 hours in children on maintenance intravenous fluids and more frequently if the results are deranged or if they are being fluid resuscitated.