Dysfunction of the central nervous system (CNS) can present as either a reduction in consciousness or with a focal neurological deficit.
Focal neurological deficit can be due to injury, infarction, haemorrhage, mass effect or infection affecting one part of the cerebral cortex (e.g. cerebral abscess). A specific region of the body is affected, resulting for example in a weak limb, paraesthesia etc.
A reduced level of consciousness can be assessed with either the AVPU scale or the Glasgow Coma Scale (GCS), which are explained later.
Agitation or confusion can be non-specific signs secondary to cerebral irritation, of which there are a number of causes.
More information may have to be obtained from any witnesses or relatives to establish the cause for a reduced level of consciousness e.g. speed of onset, incontinence of urine, history of diabetes, alcohol/drug use or history of trauma.
Assessment of the A, B and C should be made before moving on to D. The following is not a comprehensive list (as this was covered earlier) but these are specific to patients with decreased conscious level.
Airway
Breathing
Circulation
Disability

AVPU is a simpler and quicker alternative to the GCS where the patient scores A, V, P or U according to their response to stimulation. The benefit of this system is that it is clearly descriptive, giving an immediate understanding of the patient’s conscious level.

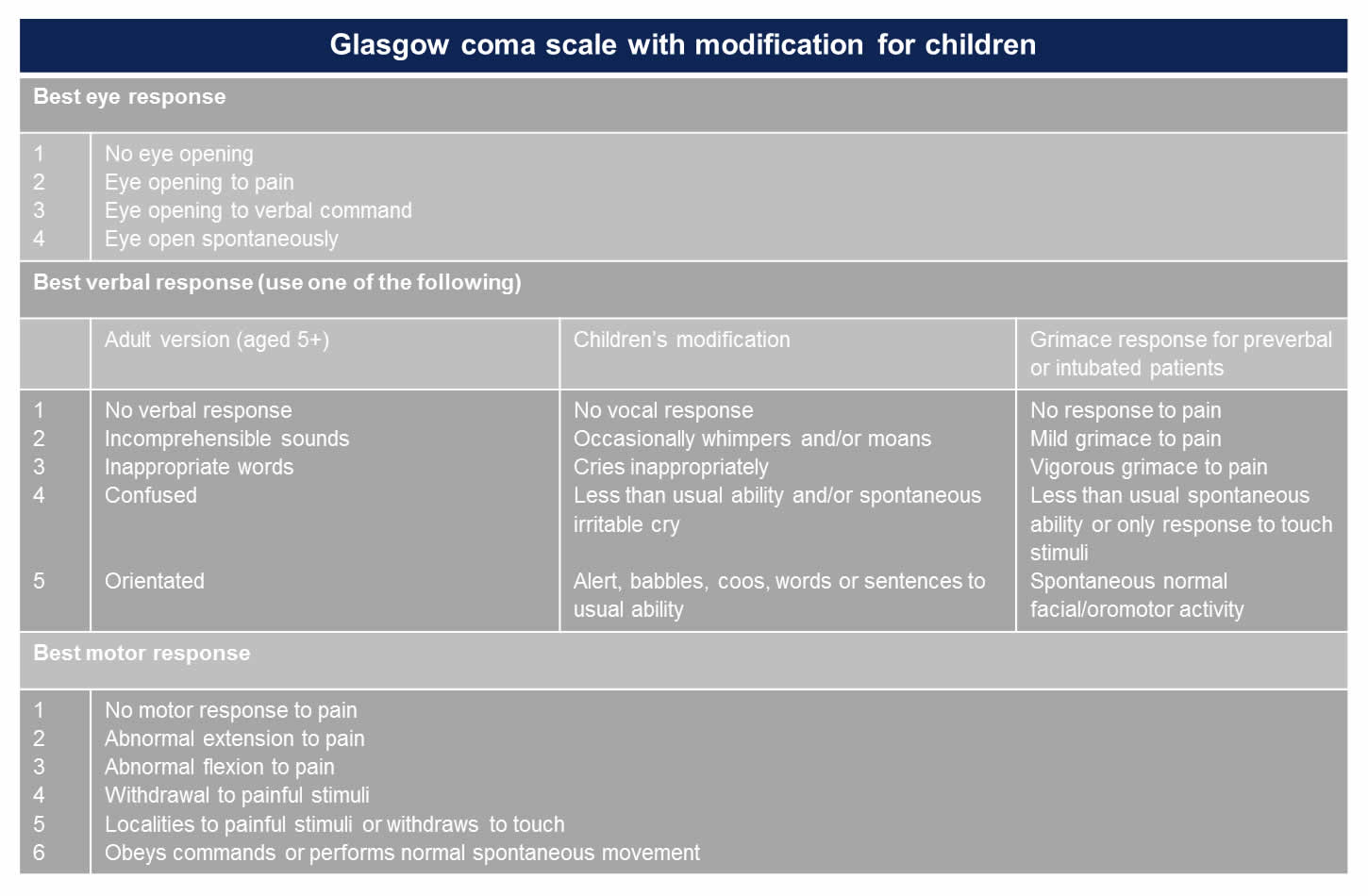
The GCS is relatively easy to perform and is a simple grading system of a patient‘s level of consciousness. There are 3 component parts, Eyes, Verbal and Motor responses to stimulation. GCS is a more complex assessment in children as their responses are often erratic even when conscious, also the scoring system is dependent on the age of the child.
When examining the pupils note the size, equality and reaction to light.
A fixed dilated pupil in the context of a brain injury indicates herniation of the temporal lobe through the tentorial hiatus (‘coning’) as a result of 3rd cranial nerve compression. Urgent discussion with a neurosurgical centre is required.
Bilateral fixed dilated pupils are a sign of brain death but can occur in hypothermia, severe hypoxia, during and post seizure, anticholinergic overdose and in deep unconsciousness.
Small reactive pupils can be seen in metabolic disorders.
Pinpoint pupils are seen with an opioid overdose and organophosphate ingestion.
The posture at rest/without stimulation may be abnormal. For example the seriously ill child may be hypotonic (floppy). A painful stimulus should be then applied. This may elicit abnormal stiff posturing:


Both hypo and hyperglycaemia can cause a change in level or consciousness and neurological functioning. The blood glucose should be measured as part of your assessment of D. A rapid finger-prick bedside testing method can be used.
Video: measuring a blood glucose
Make note of any seizure activity: when did it begin, what movements are present (of limbs, trunk, face and eyes).
Reduced consciousness due to a traumatic head injury is usually evident from the history, however, you should always look for signs of trauma which may have been overlooked. Soft tissue damage such as bruising and swelling should be looked for particularly on the back of the head, which may be hidden from view. Leaking cerebrospinal fluid (CSF) from the nose or ear is indicative of a base of skull fracture. Typically an extradural haematoma presents with a reduction in consciousness after a delay, or a lucid period following a head injury.

An unconscious patient can be managed in the lateral recovery position as long as the A, B and C are adequate. This is to protect the airway in case of vomiting if the patient does not have a protected airway such as an endotracheal tube.