It is 9pm. You are an FY1 and it is your first evening covering paediatrics. You are fast bleeped to the paediatric ward. The registrar is currently with another sick child in the emergency department. On arrival the nurse presents the case to you.
S
Hello, are you the paediatric junior doctor? Thanks for coming so quickly. I’m Helen the nurse looking after Harjit.
B
This is Harjit Singh. He’s a 4-year-old boy who was admitted earlier this evening for observation following a history of a possible seizure at home. He previously had a single febrile convulsion when he was 2 years-of-age but is otherwise normally fit and well.
A
Harjit started fitting approximately three minutes ago. He has always maintained his own airway and continues to do so. He’s breathing and maintaining his oxygen saturations at 92% on air. As you can see he is shaking all four limbs. I’ve just checked his blood sugar level and it’s 4.5mmol/l. I haven’t yet done a full set of observations.
R
Thank you for coming. Is there anything you’d like me to do?
Q – What would you like the nurse to do (RESPONSE) whilst you are on route?
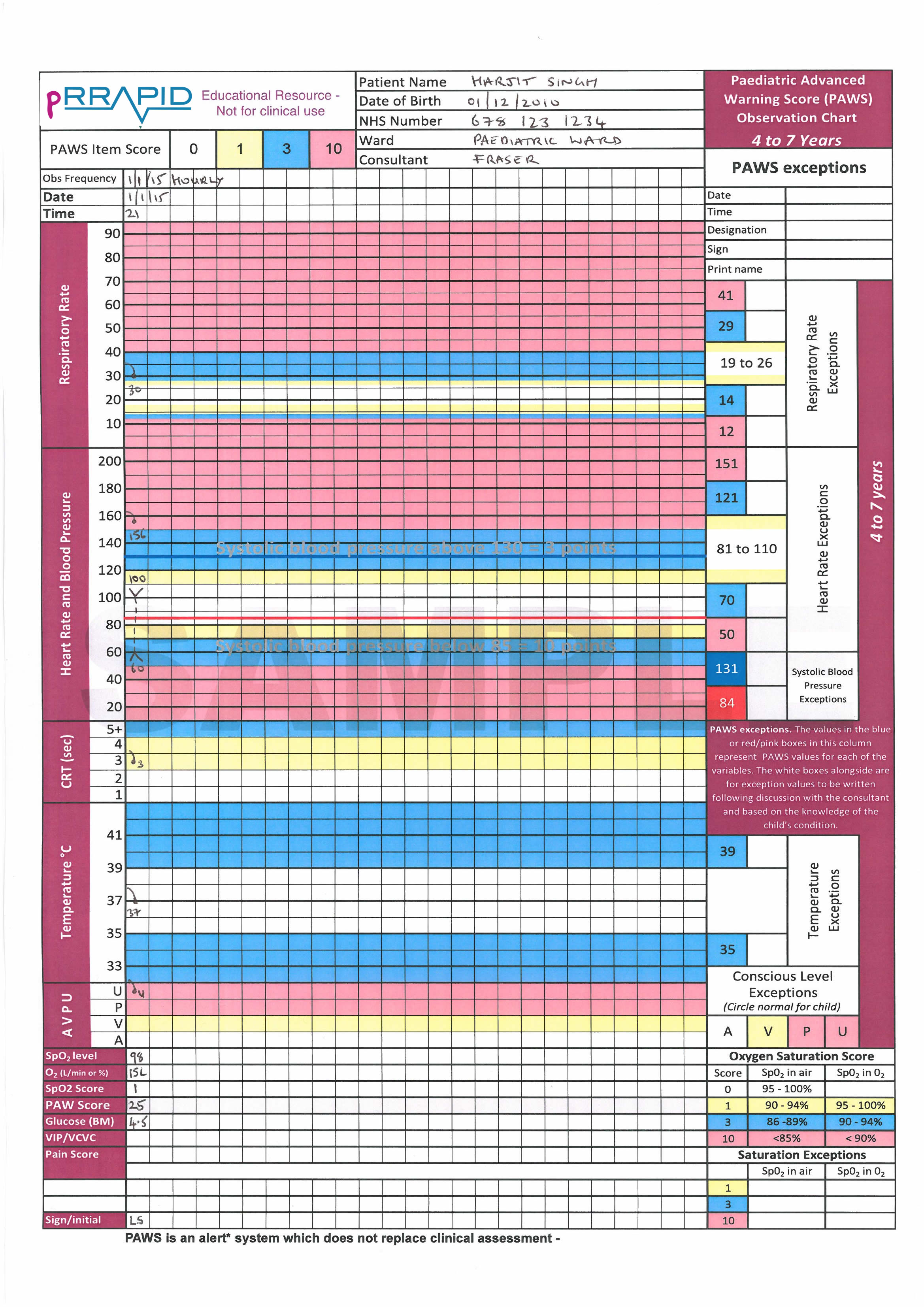
On arriving to the paediatric ward you start to assess the patient using the ABCDE approach. A full set of observations have been documented on a Paediatric Early Warning Score chart.
![]() Download PDF of Paediatric Advanced Warning Score (PAWS) chart (1.1MB)
Download PDF of Paediatric Advanced Warning Score (PAWS) chart (1.1MB)

As you approach you see that Harjit is still having a tonic-clonic seizure. The nurse tells you he has been fitting for 5 minutes now so he has just administered the buccal midazolam as you suggested.
Q – Recognition: How will you assess if the airway is patent
You assess airway patency by:
• looking for chest and/or abdominal movement,
• listening for breath sounds and
• feeling for expired air.
You are reassured to note that you can see his chest moving, you can hear breath sounds and feel the expired air. He is intermittently grinding his teeth but there does not appear to be any vomit in the airway.
Q – Respond: how do you respond?
Harjit’s airway is patent at present. There are no signs of airway obstruction and you can therefore put him into a recovery position to protect his airway and move on to breathing.
Q – Recognition: How will you assess his breathing?
You find it difficult to assess his breathing due to his tonic-clonic seizure but you can see that he is having good chest expansion. His saturations are 98% in 15L via a non-rebreathe reservoir bag. He does seem to be grunting intermittently, which you realise may be caused by the convulsion and is not necessarily a sign of respiratory distress in this instance. His respiratory rate is 30rpm.

Q – Recognition: How will you assess his circulation?
You assess circulation
He is tachycardic with a heart rate of 156 which is does not surprise you since he is fitting. His systolic blood pressure is 100mmHg. His peripheries are warm and well perfused. He looks to be of a normal colour.
The nurse informs you that he has now been fitting for 6 minutes.
Q – Respond: how do you respond to this information?

Q – Recognition: How will you assess disability?
He continues to have clonic movements of all 4 limbs. His eyes are rolling backwards, but his pupils are equal and reactive. You already know that the blood glucose was normal.
Q – Respond: how do you respond?
You continue to time the seizure, whilst you await the result of your blood gas. You are concerned that he is still fitting and ask the nurse to bleep your registrar whilst you move onto exposure.

Q – Recognition: How will you assess “exposure”?
You expose Harjit and find no further clinical signs. He is afebrile and there is no rash or bruises to find on examination.
You take a history from his father who reports that he had a “shaking episode” at home earlier today, which only lasted one or two minutes and self terminated. Other than a febrile convulsion when he was two years old he has never had seizures before. He denies any history of a head injury, recent illness or fever. He tells you that he has met all his developmental milestones, and is on no medication, nor does he have access to anyone else’s medication. Dad tells you that he himself has epilepsy.
You receive the result of your blood gas
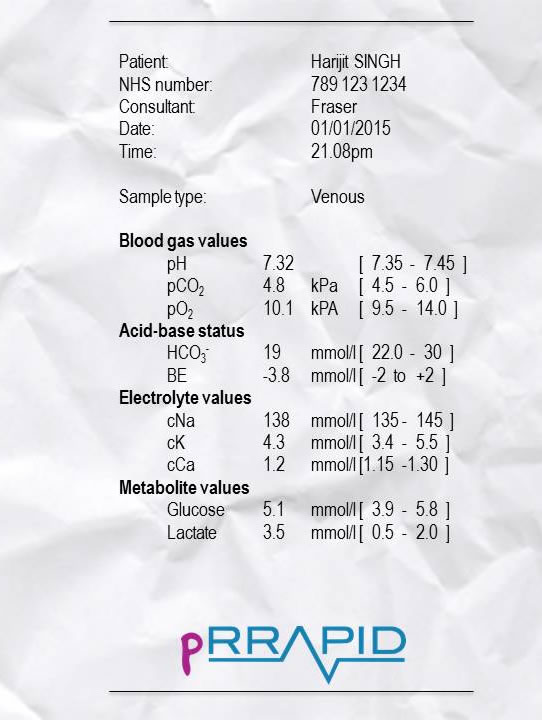
Q – Respond: What do you think is going on?
This blood gas is relatively unremarkable other than a mild metabolic acidosis with a raised lactate. These would be expected in a fitting patient (and often helps differentiate between a seizure and pseudo-seizure, with the latter having a normal lactate). This essentially normal gas tells you an electrolyte imbalance is unlikely to be the cause of the seizure, although you still await the magnesium and phosphate from the laboratory blood test.
You have already ruled out hypoglycaemia with a normal blood sugar.
There is no raised temperature at present and no history of being unwell which makes a febrile convulsion or sepsis unlikely.
There is no history of trauma or medication ingestion. His pupils are normal. A person with dilated pupils may have ingested tricyclic antidepressants (perhaps a parents medication in this case), which could lead to seizure activity. Furthermore, unequal pupils may suggest raised intracranial pressure.
The history of a seizure at home may point to an evolving seizure disorder (epilepsy) with a positive family history (dad has epilepsy too), but at present you have ruled out any reversible causes that you can treat acutely.
At this point the nurse tells you the seizure has been going on for 10 minutes since the midazolam was given (15 minutes total), and you ask him to give the 0.1mg/kg of IV lorazepam he has prepared.
The fact that Harjit did not respond to the midazolam concerns you, and you bleep your senior again for some help. Whilst waiting for you senior to call you back, you check the algorithm for status epilepticus.
The nurse asks you to prescribe the medications that have been given to this point.
Q - Please prescribe buccal midazolam.
Harjit Singh
4 years-of-age
Hospital number 123456
NHS no. 789 123 1234
NKDA
18kg
Consultant: Dr Fraser
Q - Prescribe the IV lorazepam.
Q - As two doses of benzodiazepines have not terminated seizure activity, you correctly identify that phenytoin is next on the status epilepticus algorithm. Please prescribe a loading dose of phenytoin on an infusion chart.
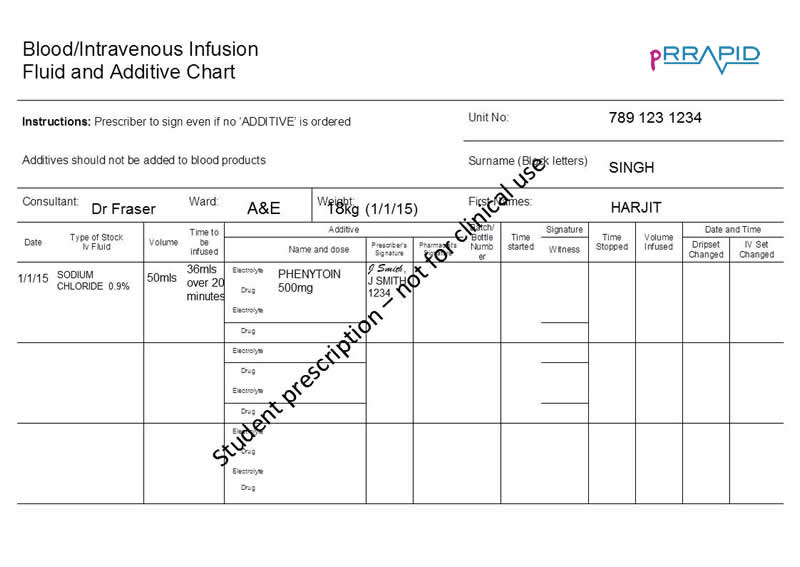
This is a hard exercise and is testing you beyond that of a medical student. Part of becoming familiar with the BNFc is being able to use the dosage section but also the “administration” section which is found just below. You will note that this asks for the Phenytoin to be diluted in Sodium Chloride 0.9%.
As you got back to reassess your ABCDE, your senior rings you back and you inform them of the patient’s condition using an SBARR structure.
S
Hi, it’s Sam here the junior doctor on for the night shift. Is that the paediatric registrar? I’m with a 4 year old boy called Harjit Singh on the paediatric ward who has been fitting for 16 minutes now.
B
Harjit was admitted for observation following a possible seizure at home. He has a history of a single febrile convulsion in the past but is otherwise normally fit and well. I understand that there is a family history of epilepsy.
A
I have assessed him – he is maintaining his own airway, is saturating at 97% with 15L oxygen non-rebreathe mask. He remains cardiovascularly well perfused, although he is tachycardic at 150. His blood pressure is normal. He has a mildly prolonged refill time (CRT) of 3 seconds. His blood glucose is 4.5mmol/l and when I inserted a cannula I took a blood gas which is essentially normal with normal electrolytes. His pupils are equal and reactive. He is afebrile.
R
He’s maintaining his own airway. I’ve placed him in the recovery position to reduce his aspiration risk.
He initially had no IV access, and we therefore gave him buccal midazolam 5 minutes after the start of the seizure. We now have access and we have just given him IV lorazepam (10 minutes after the midazolam).
I have checked the status epilepticus algorithm and I have prescribed phenytoin and have asked the nurse to prepare this. We will need to give the phenytoin in 9 minutes if he is still fitting. He has been fitting for 16 minutes now I would be very grateful if you could come and review him with me.
I am regularly reviewing his ABCD to ensure there is no change in his condition.
You document this in the patient’s notes. By the time your senior arrives the seizure has been continuing for 25 minutes and your senior asks the nurses to give the phenytoin that has prepared. Just as the anaesthetic team arrive a few minutes later, and you begin your SBAR handover again, the patient stops seizing. It is agreed by the team that he ought to undergo a CT head to rule out an intracranial cause for the prolonged seizure and be started on intravenous antibiotics to cover a potential intracranial infection.