It is 8pm. You are the junior doctor in A&E. The triage nurse calls you
Video: SBAR: Circulation (nurse)
S
Hi it’s Karen here, in triage. Is that the junior doctor? I’ve just triaged a 3-day-old patient called Callum Connors and I’m moving just about to move them to the resuscitation suite. I’d like you to review them immediately please as he’s “shutting down”
B
Callum is a 3-day old boy who was born at term in good condition by normal vaginal delivery, weighing 3kg. There were no risk factors for sepsis and he was discharged home with his mother 8 hours after birth.
A
He ‘s maintaining his own airway. He’s not tachypnoeic, but he looks grey and feels cold peripherally. He has a capillary refill time (CRT) of 4 seconds centrally and his saturations are not picking up on the saturations monitor. His heart rate is 180bpm. His blood sugar is normal. He has a raised Paediatric Advanced Warning Score.
R
Please can you come review him urgently. Is there anything you want me to do straight away?
Q – What would you like the nurse to do (RESPONSE) whilst you are on route?
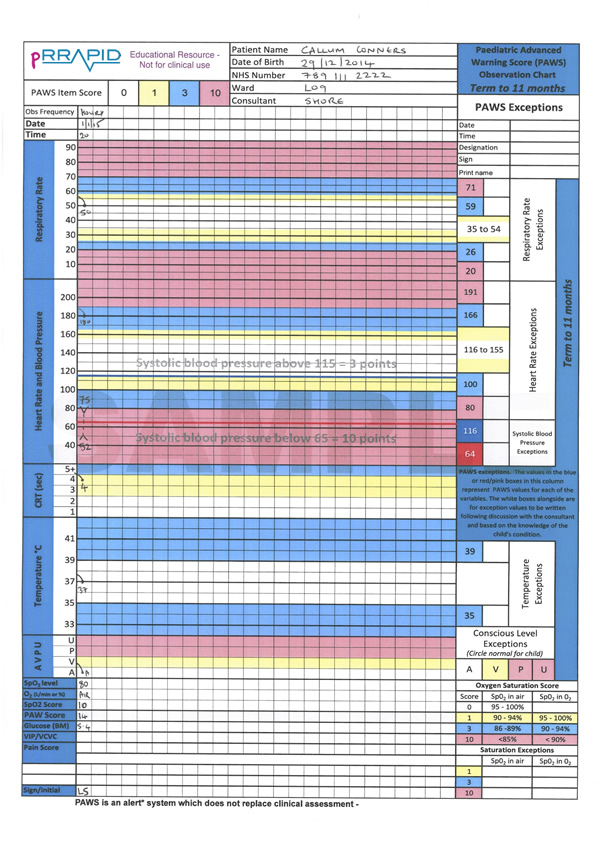
On arriving to the department you start to assess the patient using the ABCDE approach. An PAWS observation chart is available for you to review.
![]() Download PDF of Paediatric Advanced Warning Score (PAWS) chart (1.2MB)
Download PDF of Paediatric Advanced Warning Score (PAWS) chart (1.2MB)

As you approach you notice Callum is not vocalising.
Q – Recognition: How will you assess if the airway is patent
You are reassured to note that you can see his chest moving, you can hear breath sounds and feel the expired air.
Q – Respond: how do you respond?
Callum’s airway is patent and does not require an adjunct at this point. There are no signs of airway obstruction and you therefore move on to breathing.
Q – Recognition: How will you assess his breathing?
The nurse informs you that his saturations (from his left foot) were 80% in air and these do not seem to be improving with 15L oxygen via a non-breathe mask. He is tachypnoeic with a respiratory rate of 50rpm. His trachea is central and his chest is clear with no added sounds.
Q – Respond: how do you respond?

Q – Recognition: How will you assess his circulation?
You assess circulation
You feel his brachial pulse at 180bpm, but are unable to feel his femoral pulses at all. His blood pressure is 75mmHg systolic. His peripheries are cool and he looks grey. He has a central CRT of 4 seconds and a peripheral CRT of 5 seconds. His mother reports that he has not had a wet nappy for a few hours and is more drowsy that before.
Q – Respond: what is your differential diagnosis?
This infant is in unwell and there are three main differential diagnoses:
1) Sepsis: very possible and worth considering. Risk factors for sepsis include prolonged rupture of membranes (PROM) during labour, maternal sepsis during labour and maternal vaginal Group B Strep infection. This would require a history which is usually taken as part of the Exposure assessment, however in the SBAR communication the nurse informed you there were no risks for neonatal sepsis you would want to clarify this.
2) Cardiogenic shock: potentially secondary to duct-dependent congenital heart disease. The fact that the oxygen saturations do not improve with oxygen make this more likely, as well as the lack of ability to feel femoral pulses. Duct dependent cardiac lesions classically present on day 9 of life with a lactate over 10 and base deficit over 20.
3) Metabolic conditions: of which there are many. A history of consanguinity would make this more likely.
Q – Respond: how do you respond?
Q - Callum has clinical features consistent with shock. Please prescribe a fluid bolus. Remember that the cause of his shock could be cardiogenic.
Patient details:
Callum Conners,
3 days of age (you will need to create an appropriate DOB to make Callum 3 days of age.
Hospital number 7891234
NHS no. 789 111 2222
NKDA
3.2kg
Consultant: Dr Shore
NKDA
A routine bolus of sodium chloride would be 10ml/kg. This is often written up as “bolus”. In this case as a cardiogenic cause is suspected and therefore many clinicians would give this over 30minutes and then review the patient to assess if further fluid boluses are required.
As sepsis features on your differential diagnosis please prescribe Benzylpenicillin and Gentamicin (broad spectrum antibiotics for presumed neonatal infection). (Click below for information on where to find the correct medication dose)
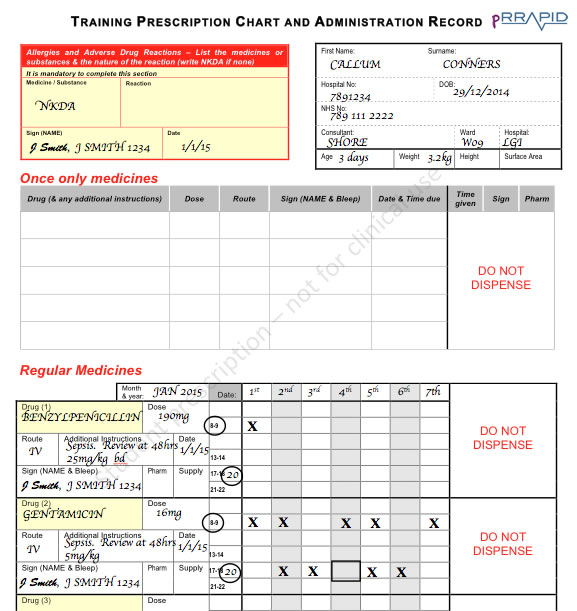
View large image
It would be appropriate to use the double dosage of benzylpenicillin (i.e. 50mg/kg) in this case. The gentamicin prescription is difficult as the medication needs to be given every 36hours. This is demonstrated with the X marks which is when the dose shouldn’t be given. The square box on the gentamicin prescription represents where a gentamicin blood level should be taken for monitoring.

Q – Recognition: How will you assess disability?
You perform an AVPU assessment and find that he does seem to be moaning intermittently but not crying spontaneously as normal. His posture is normal. His capillary blood glucose is 5.4mmol/l (normal). There is no seizure activity
Q – Respond: how do you respond?
You are satisfied that his disability is relatively stable at present so you move onto assess exposure.

Q – Recognition: How will you assess “exposure”?
You expose Callum and find no further clinical signs. He is afebrile. You are careful to minimise heat loss, as you know that heat loss in neonates can cause further compromise.
You take a history from his mother who reports that he has been fine since birth and had a normal examination by the paediatric doctor on day one of life. However, he has not been feeding as well over the last 12 hours, and seemed to become increasingly pale and drowsy over a short period of time. There is no relevant family history and mum and dad are unrelated.
You have completed your ABCDE assessment, and are extremely grateful when the paediatric emergency team arrive.
Q – Respond: how do you respond?
You hand over to them using the SBAR approach.
S
Thanks for coming. This is Callum Connors a 3-day-old boy who has just been brought into A&E by his parents with a history of becoming increasingly unwell.
B
He is a 3-day-old, term baby of unrelated parents with no risk factors for sepsis. He has had reduced feeds over the last 12 hours and has become increasingly pale and drowsy.
A
On my arrival, Callum was maintaining his own airway, but with saturations of only 80% that have not responded to 15L of oxygen via a non-rebreathe mask. He had a respiratory rate which is normal for his age of 50rpm. His chest is clear. He had a pulse rate of 180bpm with a refill time (CRT) of 4 seconds and he looked very grey on examination. I was unable to feel his femoral pulses. His blood sugar is 4.5 mmol/l and he is afebrile with no rash that I can see.
R
I’m unsure as to what is going on, but wonder if he is in cardiogenic or septic shock. We are giving a bolus of 10mls/kg of 0.9% sodium chloride, as well as intravenous Cefuroxime and amoxicillin to cover for potential sepsis. I’m about to review his response to these interventions.
Since his saturations have not improved with oxygen and I cannot feel his femoral pulses, I wonder if it is more of a cardiac problem and need further advice with management.
Your registrar agrees that that baby is cardiovascularly compromised, and with the lack of femoral pulses and poor response to oxygen wonders if this is a duct-dependent congenital heart disease such as co-arctation of the aorta. This would present itself within the first few days of life when the baby’s Ductus Arteriosus closes. She prescribes an IV infusion of Prostaglandin (5 nanograms/kg/min) which will hopefully re-open the ductus and in turn improve Callum’s cardiovascular status. She agrees with you that it was right to give antibiotics in order to cover for possible sepsis. The anaesthetic team prepare for intubation whilst the nurses prepare the Prostaglandin which should not be delayed and should be started in the A&E resuscitation room. Meanwhile, your registrar rings the Paediatric Cardiology team for further advice.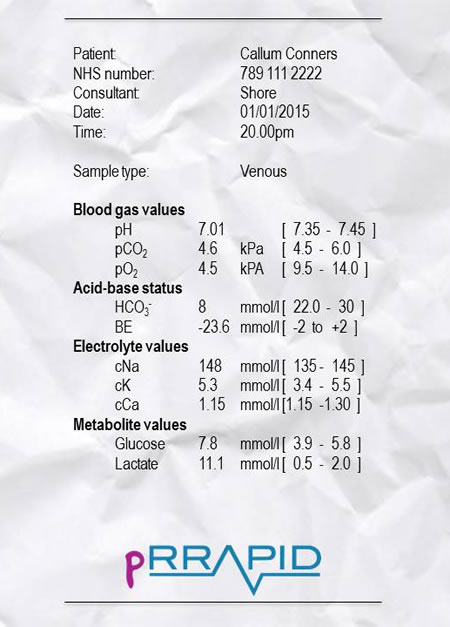
Callum’s blood gas result arrives and with the registrar you note the significant metabolic acidosis with high base deficit and high lactate.
This is a complex case and you would never been expected to manage such a case on your own. The key point is to always approach an unwell infant or child in the same methodical way using ABCDE and call for help early on.