The body normally controls the pH of blood within a tight range. One must always remember that pH is a logarithmic scale and so a change from 8 to 7 is a ten-fold increase in H+ concentration. A normal intracellular pH is required for the functioning of many enzyme systems. When blood becomes profoundly acidotic (pH<7) then cellular function becomes impossible and death ensues. There are a lot of texts available describing the causes of the respiratory and metabolic acidosis and alkalosis. However the best way to learn how to interpret blood gases is to practice.
The Advanced Paediatric Life Support Course describes a simple three step system to interpreting paediatric blood gases (do not feel you have to use this method if you already have a good system). You should always keep the Henderson-Hasselbach equation in the back of your mind whilst doing this.
CO2 + H2O = H2CO3 = H+ + HCO3-
Step 1 - What is the pH? Is there an acidosis or alkalosis?
Step 2 - What is the CO2?
If the CO2 provides a cause of the abnormal pH i.e low pH with a high CO2 (acidosis) or high pH with low CO22 (alkalosis), then the overall picture is RESPIRATORY.
If the CO2 does not provide a cause of the pH, then it is metabolic (possibly compensating).
Step 3 - Confirm your findings by looking at the base excess or bicarbonate.
If the base excess provides a cause for the abnormal pH, i.e. low pH with a negative base excess (acidosis) OR high pH with positive base excess (alkalosis), the overall picture is METABOLIC.
If the base excess does not provide a cause for the pH, it's compensating for a respiratory abnormality..

You are called to see a 8 year old child with diabetes who has diarrhoea and vomiting. Her mum reports she is drowsy and her sugars have been high. You take a venous blood gas.

Q: What is the acid-base disturbance?
Normal Blood gas.
 The only abnormal result here is the pO2, however this is a venous gas and so the pO2 should be low. This is therefore a normal blood gas. It is important to rule out a diabetic ketoacidosis in children with diabetes who are unwell with high blood sugars.
The only abnormal result here is the pO2, however this is a venous gas and so the pO2 should be low. This is therefore a normal blood gas. It is important to rule out a diabetic ketoacidosis in children with diabetes who are unwell with high blood sugars.
The learning point here is that blood gas analysis doesn’t just have to be performed on arterial blood. A lot can be established from venous or capillary samples.
A four month old baby is admitted with a cough, fever and widespread fine crackles & a wheeze. A capillary gas is taken.
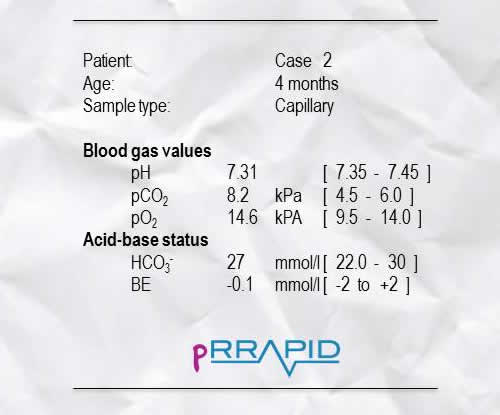
Q: What is the acid-base disturbance?
Respiratory Acidosis – Respiratory failure (bronchiolitis).
This baby has bronchiolitis. There is a respiratory acidosis. Notice the high oxygen secondary to aggressive oxygen therapy. Treatment of bronchiolitis is supportive, ie oxygen and fluids.
A 14 year old boy attends A&E. He is known to have asthma. He is short of breath, struggling to speak and on listening to the chest you can only just hear breath sounds. An arterial blood gas is taken.

Q: What is the acid-base disturbance?
Respiratory Acidosis – respiratory failure secondary to acute exacerbation of asthma
This is a respiratory acidosis. This boy is in respiratory failure secondary to an acute exacerbation of his asthma. A “silent chest” where you can only just hear breath sounds is a very serious clinical sign. This boy will need aggressive treatment and likely intubation and transfer to PICU.
A 12 year old boy has a fever, cough and right sided crepitations. An arterial blood gas is taken.
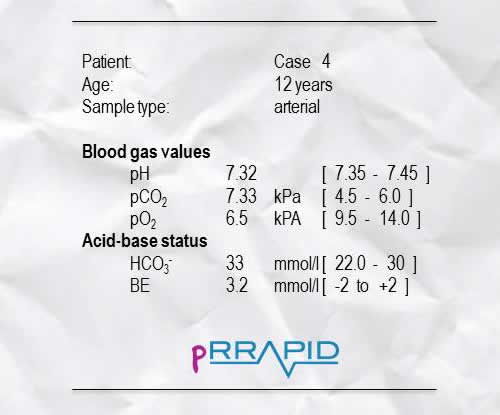
Q: What is the acid-base disturbance?
Respiratory Acidosis with metabolic compensation– Respiratory failure (pneumonia)
This boy has pneumonia associated with respiratory failure. There is a degree of metabolic compensation to his respiratory acidosis. Notice that he is also hypoxic due to the consolidated lung resulting in a ventilation:perfusion mismatch.
A 27 week gestation infant is born in poor condition. He is transferred to the neonatal intensive care unit, intubated and ventilated. A capillary blood gas is taken at 15 minutes of life
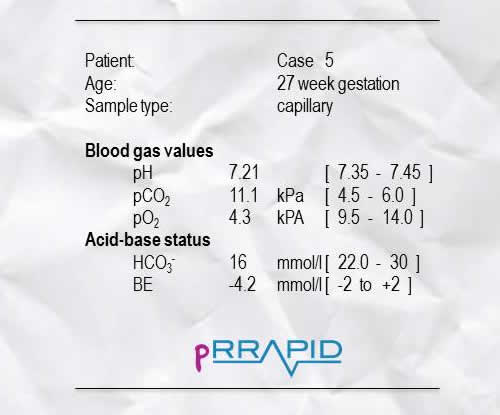
Q: What is the acid-base disturbance?
Mixed Metabolic and Respiratory Acidosis - Respiratory failure (premature neonate)
This is again a mixed metabolic and respiratory acidosis. However the significant component is the respiratory acidosis as premature newborns commonly go into respiratory failure and need ventilatory assistance. The metabolic acidosis is most likely to be due to poor peripheral perfusion but will most likely correct on its own.
A 13 year old girl has a panic attack whilst having a routine blood test. The quick thinking doctor takes a blood gas
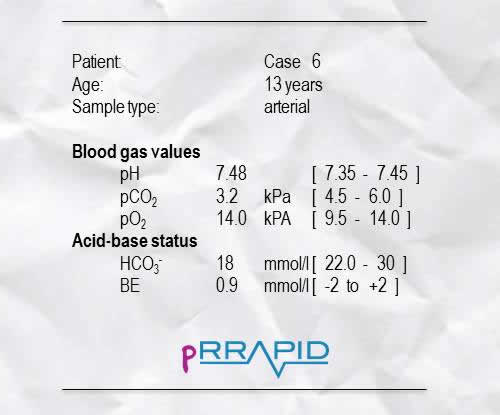
Q: What is the acid-base disturbance?
Respiratory alkalosis – Hyperventilation (panic attack)
This is a mild respiratory alkalosis. This teenager is having a panic attack and hyperventilating. The oxygen level is high due to over-breathing. A paper bag is commonly used to treat panic attacks because it allows re-breathing of the CO2 and so preventing the alkalosis. Please note that a blood gas is not a routine investigation during panic attacks. The case here is to demonstrate the blood gas changes.
You are called to see a 7 year old child with diabetes who has diarrhoea and vomiting. Her mum reports she is drowsy and her sugars have been high. You notice that she is sighing when breathing. You take a venous blood gas.

Q: What is the acid-base disturbance?
Metabolic acidosis with respiratory compensation (DKA)
This girl is most likely in DKA and has a metabolic acidosis. She is sighing as she attempts to breathe off the CO2 to compensate for the acidosis. She will need aggressive management, DKA is a life threatening complication of type I diabetes.
A five year old boy presents with a high grade fever (39.8oC) associated with a petechial/purpuric rash. His perfusion is poor (Capilary refill time, CRT, of 5 seconds). An arterial blood gas is taken.
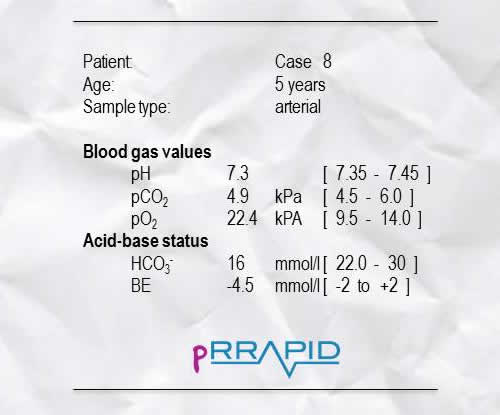
Metabolic Acidosis – Septicaemia
This boy most likely has meningococcal sepsis causing a metabolic acidosis. In this case the acidosis is relatively mild and there is no respiratory compensation. This boy will need intravenous fluids to correct his poor perfusion and intravenous antibiotics such as penicillin or a cephalosporin. Note the high oxygen level. This is because the junior doctor in A&E correctly approached this case in an ABC manner and started oxygen therapy.
Note that the acidosis is not severe. This doesn’t necessarily indicate that he doesn’t have severe disease.
A 5 week old boy presents with a four day history of vomiting. Mum describes that the vomiting has been getting progressively worse. Today he vomited out of his cot and the vomit hit the wall opposite. An capillary blood gas is taken.

Metabolic Alkalosis – pyloric stenosis
Severe vomiting causes a metabolic alkalosis by two mechanisms. Firstly there is the direct loss of hydrogen ions from the stomach. The second is the stimulation of the aldosterone system in response to hypovolaemia. This leads to salt and water retention in exchange for renal potassium and hydrogen loss and bicarbonate retention. The classic biochemical disturbance of pyloric stenosis is a hypochloraemic, hypokalaemic metabolic alkalosis.
A 13 year old girl attends A&E for treatment of a self-harm injury. The junior doctor in A&E notices pitting of the teeth. A venous blood gas is taken with an FBC.
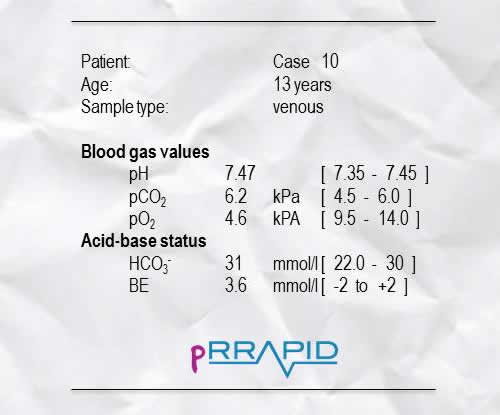
Q: What is the acid-base disturbance?
Metabolic Alkalosis with partial respiratory compensation – Bulimia
The SHO was spot on with his diagnosis of bulimia. The teeth are pitted due to chronic acid exposure. Chronic vomiting is associated with a metabolic alkalosis. The CO2 is mildly elevated suggesting a degree of compensation.
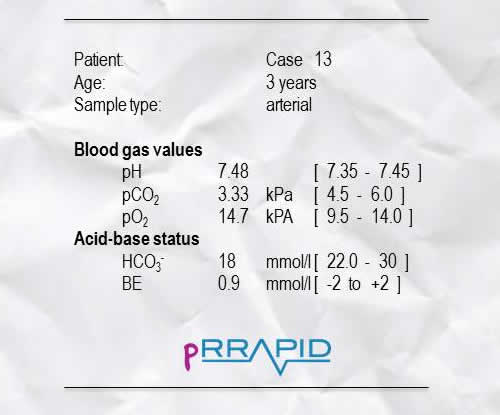
A 3 year old falls into his neighbour’s pond. An arterial blood gas is taken.
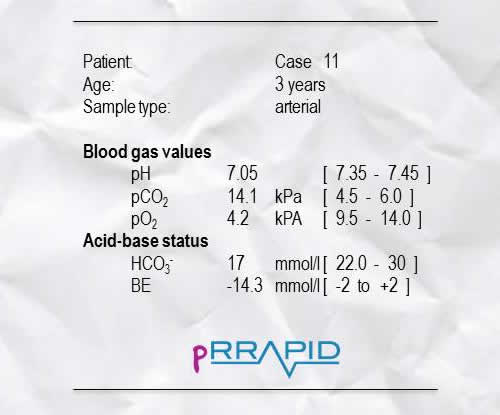
Q: What is the acid-base disturbance?
Mixed Metabolic and Respiratory Acidosis – Hypoxia
This is a mixed metabolic and respiratory acidosis. The metabolic acidosis is due to hypoxia, the respiratory acidosis due to failure to clear CO2. This is a relatively profound acidosis and this child will need aggressive resuscitation.
A three year old boy is playing in the garden when an unstable wall falls on him crushing his leg. An arterial blood gas is taken.
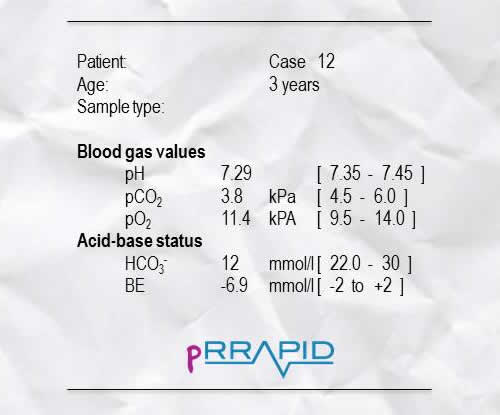
Q: What is the acid-base disturbance?
Metabolic Acidosis with partial respiratory compensation– Lactic acidosis in crush injury
This is a metabolic acidosis secondary to lactic acidosis. There is a mild degree of respiratory compensation. Lactic acid build up is caused by anaerobic respiration in the tissues of the limb where vascular supply has been compromised.
After correction of the lactic acidosis this boy develops compartment syndrome and is in a significant degree of pain. Another arterial blood gas is taken.
Q: What is the acid-base disturbance?
Respiratory alkalosis – Hyperventilation (pain)
This is a respiratory alkalosis caused by hyperventilation. This boy is hyperventilating because he is in pain. Management of pain can never be over-emphasised.
You are asked to attend a forceps delivery. The cord is round of the baby’s neck but when the baby is born he starts crying. Within a minute he is pink and self ventilating. The midwife is concerned about the cord being round the neck and so takes an arterial sample from the umbilical cord.
Q: What is the acid-base disturbance?
Erroneous result
The clinical picture doesn’t fit with the profound metabolic acidosis found here. Also if the baby was starved of oxygen then there would most likely be a respiratory component to the acidosis (raised CO2).
A 7 month old with congenital heart failure is on frusemide. A venous gas is taken.
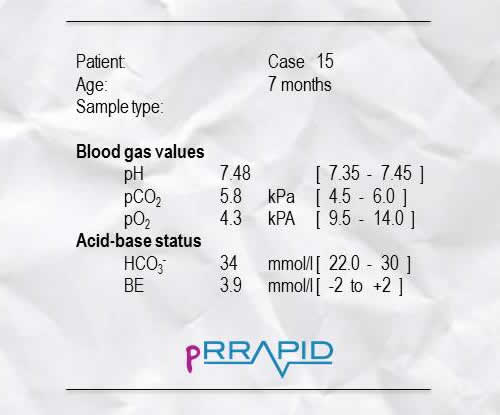
Q: What is the acid-base disturbance?
Metabolic Alkalosis – K+ deficiency (diuretic therapy)
In potassium deficiency, hydrogen ions move intracellularly to replace potassium along with loss in the urine. The shift of hydrogen intracellularly causes a metabolic alkalosis. This child needs potassium sparing diuretics included in his management.
A 14 year old boy takes an overdose of “tablets”. A venous gas is taken with salicylate and paracetamol levels.
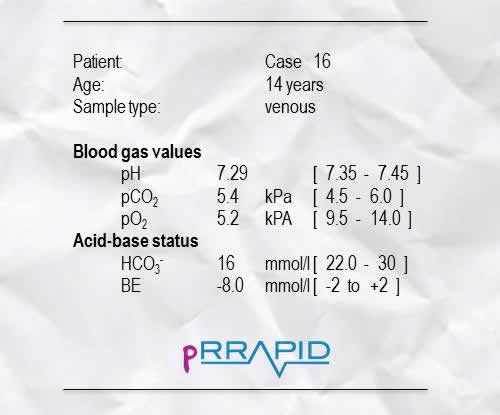
Q: What is the acid-base disturbance?
Metabolic Acidosis – Salicylate poisoning
This boy has taken an overdose of aspirin (salicylate) causing a metabolic acidosis. If this boy had presented earlier one may have found a respiratory alkalosis caused by hyperventilation (stimulated by the salicylate). This boy will need investigating with a blood glucose, U&E, prothrombin time and a serum salicylate level. Any patient presenting having taken an overdose of any kind should have a paracetamol level taken.
A 3 week old boy attends A&E. He is very unwell and the crash team is called. When you arrive the junior doctor in A&E is providing respiratory support and the senior doctor is getting access as the patient is severely hypovolaemic (CRT = 8 seconds). You “eye ball” the baby and notice a lump in his left groin. A venous blood gas is taken.
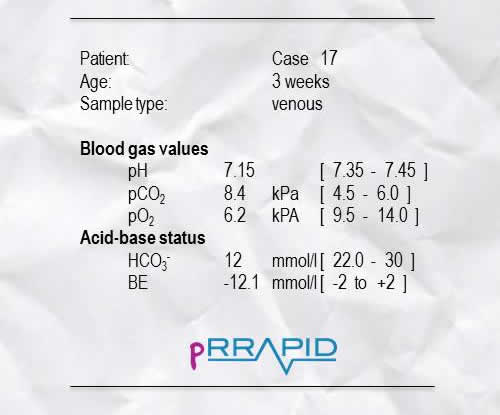
Q: What is the acid-base disturbance?
Mixed Metabolic and Respiratory Acidosis – Bowel death in incarcerated hernia
This is a mixed metabolic and respiratory acidosis. This boy had an inguinal hernia which had incarcerated. The bowel obstruction had caused bowel infarction which can cause a metabolic acidosis. The obstructed contents of the bowel were splinting the diaphragm preventing respiration and thus causing a respiratory acidosis. The hernia was corrected and a small section of bowel removed.
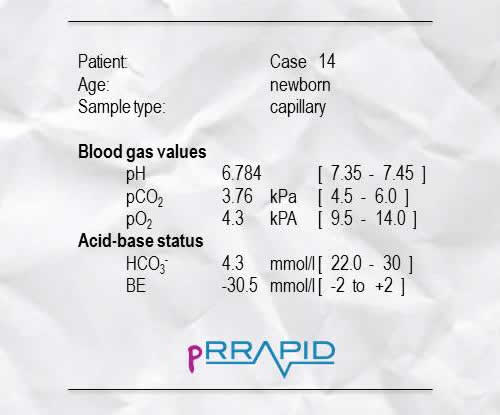
You are called to attend the delivery of an undiagnosed breech delivery. The delivery of the head was delayed and the baby was flat on delivery.

Q: What is the acid-base disturbance?
Mixed metabolic and respiratory acidosis – Hypoxia and respiratory failure.
This baby was flat at delivery and making no respiratory effort. The hypoxic episode caused by delayed delivery of the head had caused the acidosis. The baby was therefore intubated and ventilated. Within 5 minutes he had good respiratory effort and was extubated. A fluid bolus was needed to correct the metabolic acidosis. Within an hour this little baby was bottle feeding and made a full recovery.