Oxygen can be delivered through a number of devices. It's important to divide oxygen delivery into flow and concentration. This has particular implications in paediatric patients who have small tidal volumes (volume of lungs).
The volume of gas a patient inspires every minute is known as the minute volume (MV). Where:
A small infant of 3.5kg may have a MV of only 700mls/min. Therefore giving 1litre of oxygen via a nasal cannula could result in a high concentration of oxygen. A 70kg adolescent however may have a resting MV of 6l/min and therefore giving 1l of nasal oxygenation will only result in a modest increase in inspired oxygen (approximately 4% increase).
If a patient's peak inspiratory demand (minute volume) is greater than the flow delivered by the device (e.g. a simple face mask) then room air will be sucked in around the side of the mask and reduce the concentration of oxygen being delivered, this is known as "entrainment".
Equipment and Methods for Oxygen Delivery and Support of Ventilation: In resuscitation of an acutely unwell child oxygen should ideally be given immediately at a flow rate of 15 litres per minute. Different methods of oxygen delivery are used depending on the age of the child and their clinical condition.
Low-flow |
Low flow nasal cannula |
 |
Simple face-mask |
 |
|
Non-rebreathe mask |
 |
|
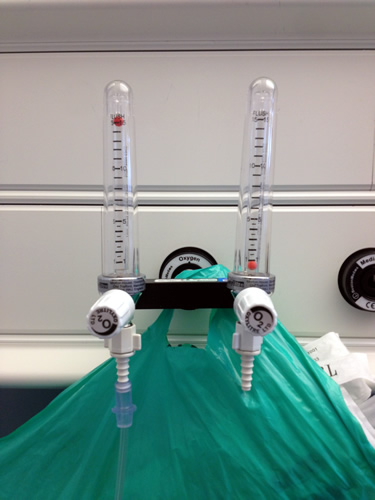
High-flow |
High flow mask. As the flow of gas delivered is very high (and therefore entrainment is unlikely) the concentration can be tightly controlled |
 |
| High flow nasal (Vapotherm) High flow of humidified gas through nasal cannula. |
 |
If the patient is not breathing (apnoeic) then it will be necessary to ventilate them. Either mouth to mask ventilation can be used (usually done in out of hospital situations) or a self-inflating bag-valve mask (BVM) device can be used. Prior to ventilation ensure that the airway is patent using the techniques described above. An obstructed airway will become obvious if attempted ventilation fails to push air/oxygen through the airway.
Patients who are not quite apnoeic but are failing to breathe enough to maintain oxygenation and carbon dioxide levels will also require ventilation.
Patients who are peri-arrest may appear to be 'gasping' or have irregular breathing. Ventilation can still be done with a bag-valve mask (BVM) device in this situation until help arrives for a more definitive plan such as intubation.
Video: Using a Bag-valve mask (BVM) device. The two person technique in a child is the same as an adult. In an infant the major variation is the neutral head position to maintain the airway.

A BVM is usually used with an oxygen source to enable children to be ventilated using a high concentration of inspired oxygen. If connected to an oxygen source they can deliver up to 50% oxygen and if a reservoir bag is also connected this allows an oxygen concentration of around 90% to be delivered. Self-inflating bags can also be used to ventilate patients with endotracheal tubes already in situ.
Two person technique for ventilating patients with a bag-mask device (see figure below)

If the patient is not breathing (apnoeic) then it will be necessary to ventilate them with a BVM device. Prior to ventilation ensure that the airway is patent using the techniques described above. An obstructed airway will become obvious if attempted ventilation fails to push air/oxygen through the airway. A self-inflating bag (e.g. AMBU® bag) is connected to a mask, which is held tightly to the patient's face to form a seal, then the bag is squeezed to give a breath. This is best done as a two-person technique with one person holding the mask and the other squeezing the bag at a rate of 10-12 per minute. Observation for chest movement is required to ensure adequate ventilation. A self-inflating bag can also be attached to an endotracheal tube if already in situ.
Patients who are not quite apnoeic but are failing to breathe enough to maintain oxygenation and carbon dioxide levels will also require ventilation. Patients who are peri-arrest may appear to be 'gasping' or have irregular breathing. If there is insufficient respiratory function then ventilation should be instigated with a BVM device until help arrives for a more definitive plan such as intubation.
Patients who vomit can aspirate fluid into their lungs. Therefore it is important to site a naso-gastric tube and aspirate stomach contents to prevent aspiration and protect the lungs. This becomes especially important when mechanically ventilating a child with a bag-valve mask (BVM) device, as the stomach will be filled with air. A stomach full of air can cause splinting of the diaphragm making ventilation more difficult. Therefore use a nasogastric tube to decompress the stomach, once the airway and ventilation have been established.