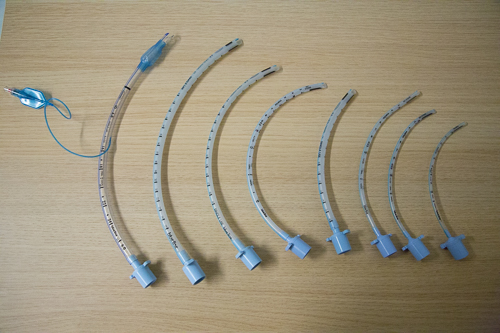
If the patient is unable to protect their own airway,i.e. reduced conscious level prevents adequate cough or gag, then a definitive airway (endotracheal tube) will be required. A GCS ≤8 or a rapidly falling level of consciousness is an indication for a definitive airway. Call for anaesthetic help.
Anaphylaxis is a serious and life threatening condition which occurs secondary to an immunologically mediated reaction to various allergens. Histamine release causes angioedema and bronchospasm resulting in significant airway compromise. It can also result in capillary leak leading to shock. There is a variable clinical presentation but it is normally characterised by a rapid deterioration with rash and life threatening airway, breathing and circulatory problems. Airway signs can include stridor and wheeze and signs of circulatory involvement include hypotension and tachycardia. Severe anaphylaxis can result in respiratory or cardiac arrest. Treatment is covered in the Medical Emergencies chapter.
Epiglottitis is inflammation of the epiglottis, which as a consequence can enlarge and cause airway obstruction. Bacterial infection is the most common cause, occurring most commonly in children 2 to 4 years-of-age. The incidence has decreased since the introduction of the Hib vaccine against Haemophilus influenza. Be particularly suspicious of epiglottitis as a cause of stridor in unimmunised children.
Children with epiglottis present with a sudden onset stridor associated with fever, pallor and drooling. The drooling is due to inability to swallow their oral secretions. If you suspect epiglottitis it is imperative that you DO NOT ATTEMPT TO EXAMINE THE THROAT as this could cause complete airway obstruction (this is true also for cases of bacterial tracheitis and croup). Also do not attempt to cannulate, give nebulised medications, or perform neck radiographs. Instead contact a paediatric anaesthetist who will be able to perform an intubation under controlled conditions. After an endotracheal tube has been placed, the underlying cause can be treated with intravenous antibiotics.
Croup is characterised by a barking “seal-like” cough and inspiratory stridor. It can be viral or bacterial with parainfluenza virus being the most common cause. Croup tends to affect children between 6 months and 4 years and is most common during the winter months. It is usually a self-limiting illness but can often cause more severe symptoms requiring intubation. It tends to respond well to steroids and the need for steroid treatment is decided based on the modified Westley Croup Score.
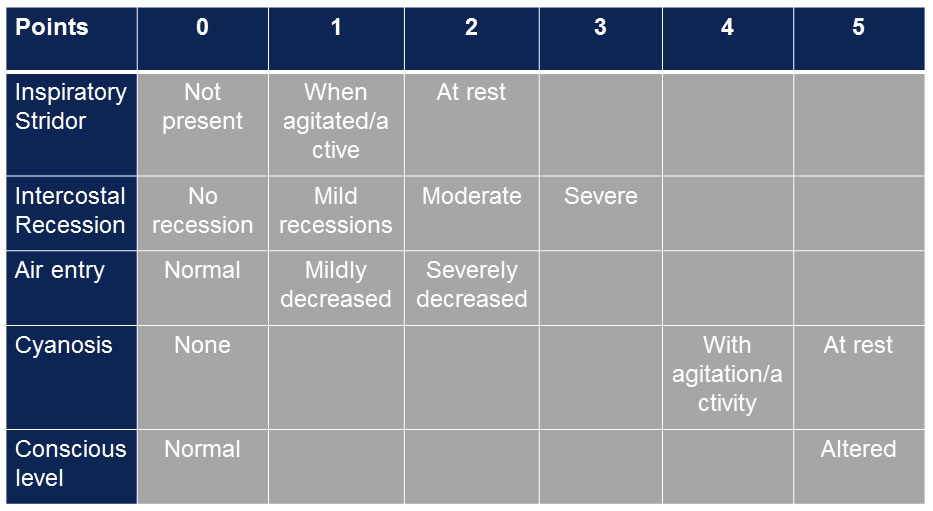
In mild croup usually just observation is needed but if moderate or severe you will need to treat with oral dexamethasone and potentially nebulised budesonide or adrenaline if worsening.
In the case of foreign body obstruction and severe respiratory distress in the first instance it is important to initiate the “choking child” procedure (in the BLS section). If this is unsuccessful a laryngoscopy will need to be performed. It is important throughout the management of a child with foreign body aspiration that you do not cause any further distress that may precipitate complete airway obstruction.