Video: SBAR, Airway (Nurse)
S
It's Helen here the nurse in A&E triage, is that the junior doctor? Hi, I've got a child in triage that I'm moving to the resuscitation room. I'd like you return to review him please as he has noisy breathing and significant difficulty in his breathing.
B
The patient is Aaron Johnston who is a 2-year-old boy who is normally fit and well. He has had a barking cough for two days, but since early this morning his mother has noticed that he is making loud noises when he breathes.
A
I've examined him briefly and he has a stridor at rest. He seems to be working very hard to breathe, has saturations of 90% and has a respiratory rate of 44rpm. His paediatric early warning score is raised.
R
I'd really like you to come and review him immediately please. Is there anything you'd like me to do whilst you are on your way?
Q – What would you like the nurse to do (RESPONSE) whilst you are on route?
An observation chart (PAWS) has been completed for Aaron
On your arrival back to A&E, you start to assess the patient using the ABCDE approach.

As you approach you notice that Aaron is sat on his mum's lap, making loud inspiratory noises. At present he is not talking.
Q – Recognition: How will you assess if the airway is patent
Click below to see your clinical findings
You can hear a harsh inspiratory stridor as you approach Aaron, with an intermittent barking cough. You are pleased that you can see his chest moving and can hear breath sounds and feel expired air.
Watch the video below or at: https://www.youtube.com/watch?v=Wvg7HFoKFtY
VIDEO: Severe Respiratory Distress
Video courtesy of Damian Roland. This video is also available at: https://www.youtube.com/watch?v=Wvg7HFoKFtY
Q – Respond: how do you respond?
The harsh stridor alerts you to the fact that his upper airway may be partially obstructed. You are particularly concerned that he is having stridor at rest and ask the nurse to bleep the paediatric registrar as well as the anaesthetic team whilst you continue to assess the patient, so that they can provide assistance if his condition deteriorates.
Q – Recognition: How will you assess his breathing?
Click here to see your clinical findings
The nurse informs you that his saturations were 90% in air when he arrived but with the non-rebreathe oxygen mask placed close to his face they are now 95%. She tells you that he doesn't tolerate the oxygen mask too close to his face and his distress makes his breathing worse so she has asked mum to hold it near his face. You are aware that an oxygen requirement in the presence of acute airway obstruction is a worrying sign.
He is tachypnoeic with a respiratory rate of 44rpm. His trachea is central, however he has significant intercostal and subcostal recessions with tracheal tug.
He has reasonable air entry throughout his chest, but this is dampened on auscultation by transmitted sounds from his loud stridor.
Q - At this point what are the most likely differential diagnoses, and why?
Croup is the most likely diagnosis given the two day history of a barking cough. This diagnosis is common in Aaron's age group, and the worsening of symptoms at night is classical.
Bacterial tracheitis is a life threatening form of croup and is an important differential for croup. Bacterial infection of the trachea results in purulent secretions, with the child appearing septic with a high fever. The absence of drooling and presence of a cough helps to distinguish this from epiglottitis.
Epiglottitis is an important differential diagnosis as the airway obstructs more frequently than in croup, but the child often presents with a short history of stridor and drooling due to not being able to swallow secretions. They may have a muffled voice. They are often septic in appearance. Thankfully due to national immunisation programmes epiglottis is now rare, and therefore bacterial tracheitis is a more likely differential.
Foreign body is also an important differential to consider and the parent/carer may have witnessed a choking episode. This usually presents with a sudden onset history and unilateral signs on examination.
Anaphylaxis may also present with stridor but would usually have a precipitating factor (e.g. eating nuts) rather than simply occurring whilst the child was asleep. Additionally lip/tongue swelling with an urticarial rash is often present in anaphylaxis.
Q – Respond: how do you respond?
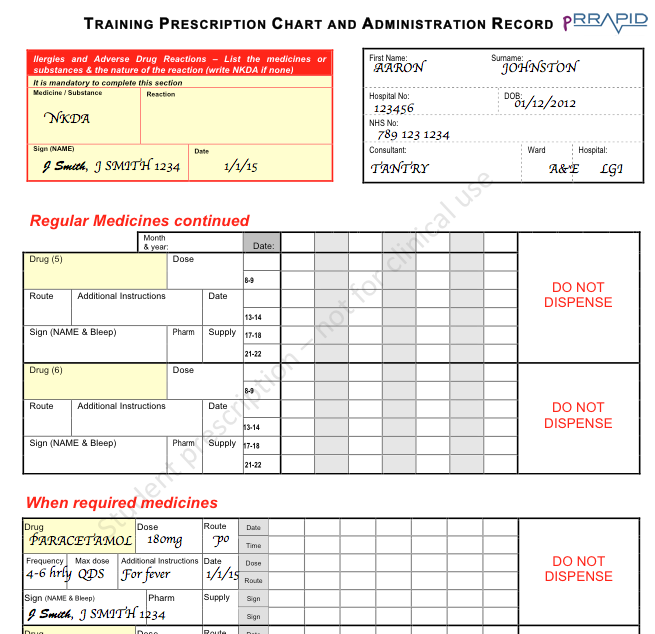
Patient details:
Aaron Johnston,
2 years old.
Hospital number: 123456
NHS no. 789 123 1234
NKDA
Consultant: Dr Tantry
Q – What is his estimated weight
1-12 months = (0.5 x age in months) + 4
1-5 years = (2 x age in years) + 8
6-12 years = (3 x age in years) + 7
Therefore predicted weight of 12kg .
Q - Use a blank pRRAPID prescription chart (or local prescription chart) and prescribe an adrenaline nebulizer. NB you can make up a date of birth to make Aaron 2 years of age. (Click below for information on where to find the correct medication dose)
Throughout the e-book you will be asked to undertake a series of prescribing exercises on both drug charts and fluid charts. More information is included in the Prescribing Chapter. You can perform these on the drug chart that is used in your local hospital or on our RRAPID drug and fluid charts. These have been designed specially for this e-book and should not be used for clinical work.
Download Drug chart
Download Fluid chart
You are aware that nebulized adrenaline results in only a transient improvement in airway obstruction. 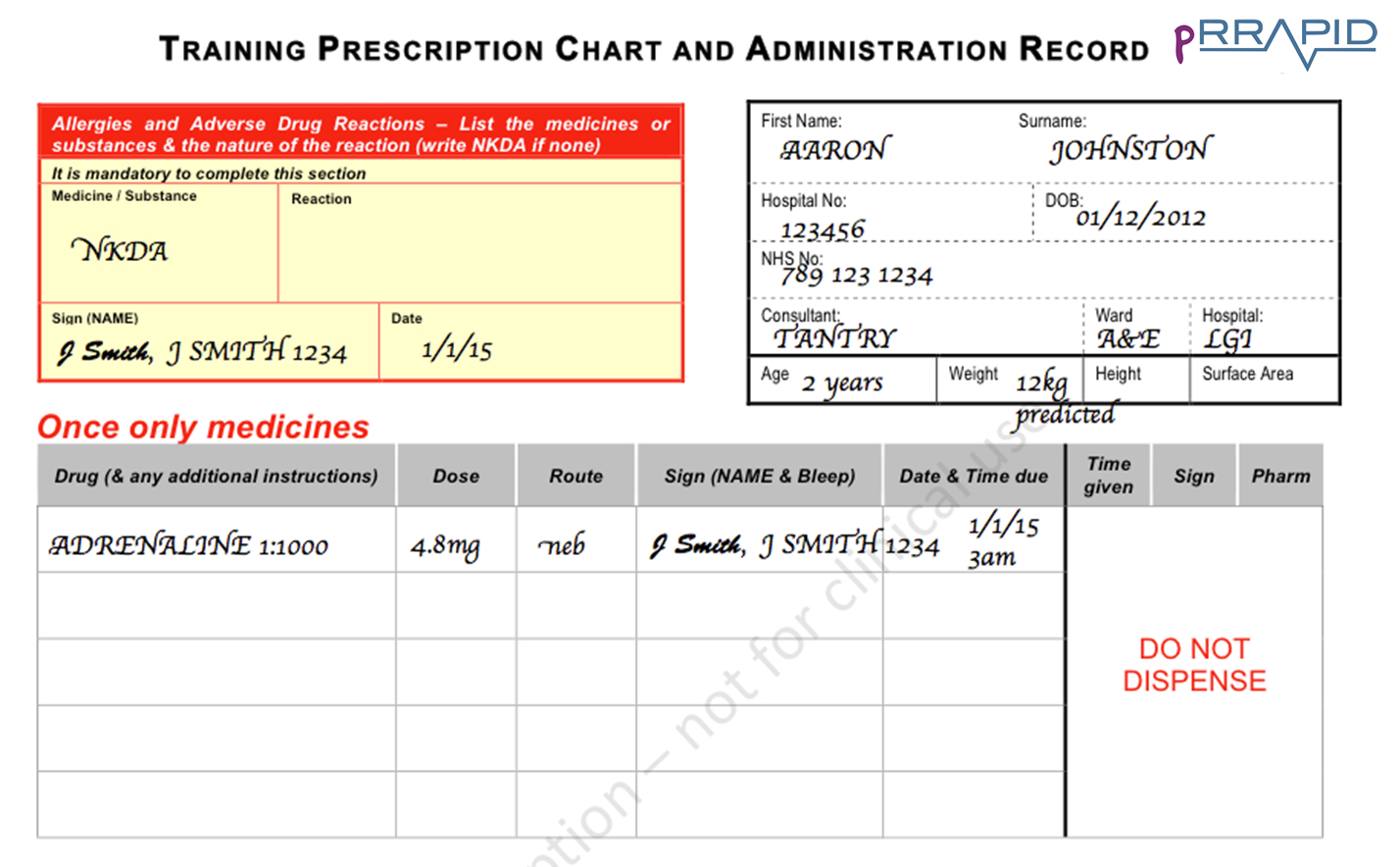
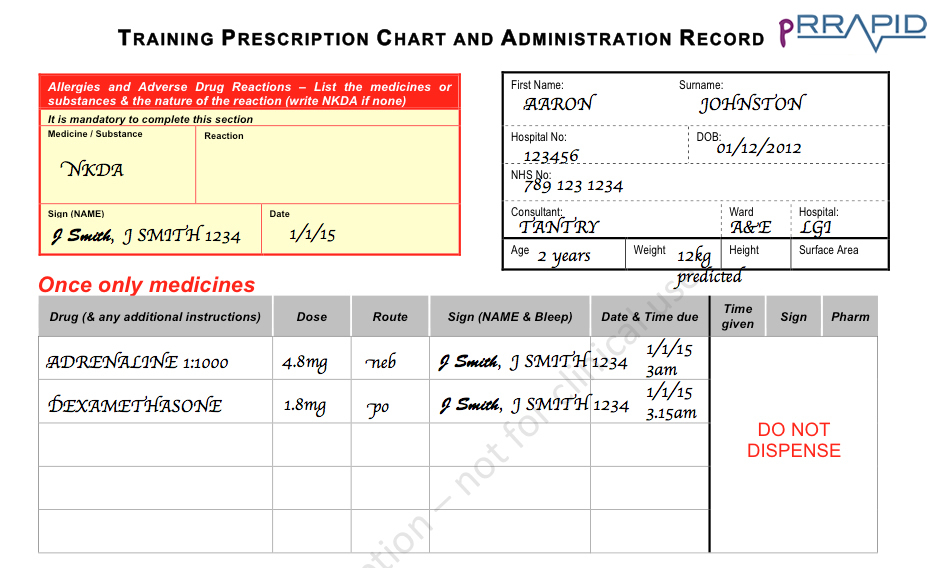
Q – Respond: is there any other treatment you could give him?
Yes – you could also give him oral dexamethasone or nebulised budesonide (a steroid), both of which can be repeated after 12 hours. However, giving nebulised adrenaline first in this situation is the priority, as it will improve his symptoms the fastest. It would be reasonable to consider giving a combination of both oral and inhaled steroid (dexamethasone and budesonide) in severe cases to ensure absorption/action.
You decide that he will also need steroid therapy. He is drinking fluids, you therefore chose to give oral Dexamethasone.
Q – Using your pRRAPID prescription chart, prescribe a single dose of dexamethasone.
Q – Respond: you wonder if there are any further investigations you should do?
No. In a child with stridor, and in turn a potentially compromised airway – it is best to avoid upsetting the child any further. Performing blood gases or chest x-rays are unlikely to contribute to assisting your diagnosis at this stage, and are in fact are more likely to upset the child and make the airway compromise worse.
You should however continue to monitor oxygen saturations, particularly to assess response to the adrenaline nebuliser.
Whilst the nebulised adrenaline is running, and the nurse is preparing some dexamethasone, you move on to assess his circulation.

Q – Recognition: How will you assess his circulation?
You assess circulation
He is tachycardic with a heart rate of 150. The pulse volume is normal. His peripheries are warm and he has CRT of less than 2 seconds. You are unable to get a blood pressure as he becomes distressed when the blood pressure cuff is placed over his arm and so you decide not to check it at present. He remains alert, and mum says he passed urine through the night.
Q – Respond: how do you respond?
You feel that his circulation is stable at present, and you are concerned that inserting a cannula may distress him further so you decide to just monitor him and move on to assess disability.

Q – Recognition: How will you assess disability?
Click here to see your clinical findings
You perform an AVPU assessment and note that he is fully alert and looking around. His pupils are equal and react to light. His posture is normal. You do not perform a blood sugar at this point as doing so could cause him distress and compromise his airway.

Q – Recognition: How will you assess “exposure”?
Click here to see your clinical findings
You expose Aaron and find no further clinical signs other than a temperature of 38.0o Celsius.
You take a history from his mother who reports that he has been very snotty with temperatures for the last 2 days, but his breathing seemed to get much worse overnight. She tells you that his immunisations are up-to-date and he has no other medical problems.
Q – Respond: Why is immunization history important in this case?
As discussed above epiglottis is an important differential in cases of stridor. Epiglottitis has thankfully become more rare since the Haemophilus influenzae vaccine. It is always worth identifying immunisation status as such information may aid your diagnosis.
Q – Respond: What do you do now?
S
Hello, it's Michael, the junior doctor from A&E here, is that the paediatric registrar? I'm currently in resuscitation room and I've just seen a 2 year old boy called Aaron Johnston who presents with stridor and difficulty in breathing who I would like you to review please.
B
Aaron is normally fit and well, but has had a two day history of a barking cough and fever. He started having difficulty in breathing today.
A
He initially had audible stridor at rest, had considerably increased work of breathing with a respiratory rate of 44rpm with oxygen saturations of 90% in air. I have given him a dose of nebulised adrenaline and a dose of oral dexamethasone. He now has oxygen saturations of 97% on flow by oxygen at 15l. His stridor has improved following the adrenaline nebuliser. He is tachycardic at 150bpm, but his cardiovascular status is otherwise stable although I haven't got a blood pressure as he seems to become distressed when we try. He is alert and responsive, but febrile with a temperature of 38o Celsius.
R
I think he has croup. I am happy that he is relatively stable at present but am wary that the effect of the adrenaline will only last a short while and so I would be grateful if you could attend to review the patient with me. I have also bleeped the anaesthetic team who I'm told are on their way.
You document this in the patient's notes and review the patient with the paediatric registrar and anaesthetic team, who have decided that this child may be a candidate for intubation if his clinical status deteriorates.
Q – Respond: When would tracheal intubation be necessary?
The decision to intubate is a clinical one based on worsening tachycardia, tachypnoea and chest recessions, or cyanosis, exhaustion or confusion. Less than 5% of children admitted to hospital with croup require tracheal intubation.
Q - Aaron is febrile and not had any antipyretics in the last 8 hours. Please prescribe an appropriate dose of paracetamol.
Aaron has an illness that may require him to have an anti-pyretic given whilst in hospital. As it is currently not needed to give this medication regularly four times a day it should be prescribed on the “when required” (PRN) section of the prescription chart as shown here. Anti-pyrexial medications, such as paracetamol and/or ibuprofen, are commonly prescribed for children in hospital. However, they do not need to be used with the sole purpose of bringing down a fever.