- “Life-threatening organ dysfunction caused by a dysregulated host response to infection”(The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3) JAMA Feb 23, 2016 Volume 315 Number 8)
- NICE guidance highlights (NICE guidance NG51)
- Children under 1 year of age
- Adults over 75 years old
- People who are very frail
- People who are immunocompromised
- Patients post-surgery
- People with any damage to the skin such as burns, blisters, wounds
- Intravenous (IV) drug users
- People with lines or catheters
- If possible, ascertain:
- How the patient is feeling
- What symptoms they have
- Do they have any allergies
- Cough
- Shortness of breath (dyspnoea)
- Cyanosis
- Pale
- Clammy
- Sweating
- Cool peripheries
- Fever
- Rigors
- Dysuria
- General Signs
- Tachypnoeic
- Low oxygen saturations
- Delayed capillary refill time
- Reduced skin turgor
- Dry mucous membranes
- Hypotensive
- Tachycardic
- Decreased urine output
- Severity
- Initial Assessment and Investigations
- ABCDE assessment
- Assess patient’s airway
- Monitor oxygen saturations and respiratory rate
- If patient is hypoxic give Oxygen (O2) to achieve target saturations. Initially give 15 L/min via a reservoir mask if the patient is acutely unwell
- Target saturations:
- 94 - 98% for patients not at risk of hypercapnic respiratory failure
- 88 - 92% for patients at risk of hypercapnic respiratory failure due to conditions such as Chronic Obstructive Pulmonary Disease (COPD)
- Examine patient’s chest
- Listen for:
- Asymmetric breath sounds,
- Crepitations
- Increased resonance
- Pleural rub
- Listen for:
- Arterial blood gas (ABG) if concerned about patient’s ventilation
- Chest X-ray if concerned about the patient’s ventilation. If the patient is unwell request a portable X-ray
- Obtain intravenous access by placing 2 large bore cannulae in the antecubital fossa. Take blood to check Full Blood Count (FBC), Urea and Electrolytes (U&Es), Liver Function Tests (LFTS), Venous Blood Gas (VBG), Blood Cultures, C-Reactive Protein (CRP) and Clotting
- Check Capillary Refill Time (CRT) - hold for five seconds and refilling should occur in 3 seconds
- Assess pulse rate, rhythm and character
- Monitor heart rate and blood pressure
- Intravenous (IV) fluid bolus of 0.9% sodium chloride 250-500 ml over 10-15 mins as required by clinical picture and balanced with patients’ risk of fluid overload.
- See more details in the “Circulation” Chapter in the “Response” Section under “Fluid Challenge”
- Listen to patient’s heart sounds
- Check urine output and consider catheterisation
- Check pupils are equal and reactive
- Assess Glasgow Coma Scale or ACVPU using the NEWS2 chart
- Check patient’s temperature and blood sugar
- If suspicion of sepsis ensure Sepsis 6 care bundle is completed (a useful neumonic for this is BUFALO)
- B - take Blood Cultures
- U - start Urine output monitoring/check U+E/Urinalysis and urine cultures if positive
- F – Start Intravenous Fluids if not already done so
- 0.9% Sodium Chloride 500 ml over 10-15 minutes. See more details in the “Circulation” Chapter in the “Response” Section under “Fluid Challenge”
- A – Start Broad Spectrum Antibiotics
- L – Check the Lactate (venous gas)
- O – Apply Oxygen if not already done
- Examine patient’s abdomen and legs
- Consider venous thromboembolism prophylaxis
- Call for senior help if not done already
- Management
- Immediate pharmacological management
- Start antibiotics as per trust guidance
- Referrals
- Discuss with senior member of the team
- Contact critical care outreach team
- Consider referral to Intensive Care Unit (ICU) if:
- Failure to respond to medical management
- Patient requires ventilator support
- Patient requires blood pressure support
- Deterioration of blood gas despite full medical management
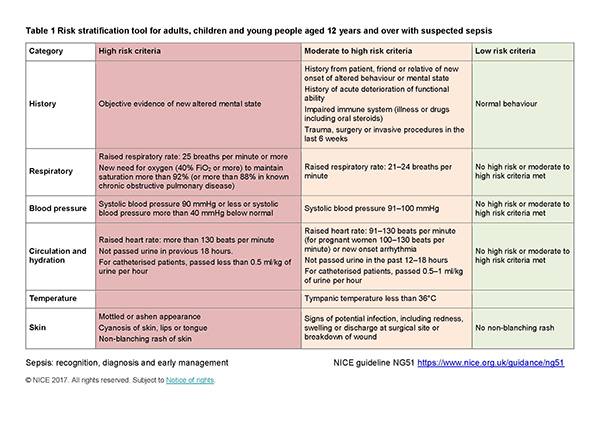
NICE Risk stratification tool for adults, children and young people aged 12 years and over with suspected sepsis