Recognition
- Paracetamol is a common drug to take in an overdose. If it is treated early, recovery is usually excellent, however in delayed presentation it can lead to Liver failure and death
- Time of overdose
- Dosage
- Single ingestion or staggered overdose
- Was it a mixed overdose
- Any other regular medications or alcohol
- Intent (accidental vs self-harm)
- Initially mild and non-specific
- Delayed signs:> 24 hrs
- Abdominal pain particularly right upper quadrant pain
- Nausea and vomiting
- Jaundice
- Reduced GCS
- Deranged LFTs
- Coagulopathic
- Renal failure
- Hypoglycaemia
- Lactic acidosis
- ABCDE assessment
- Sit patient up if able to tolerate
- Assess patient’s airway– call an anaesthetist if airway compromised
- Monitor oxygen saturations and respiratory rate
- If patient is hypoxic give Oxygen (O2) to achieve target saturations. Initially give 15 L/min via a reservoir mask if the patient is acutely unwell
- Target saturations:
- 94 - 98% for patients not at risk of hypercapnic respiratory failure
- 88 - 92% for patients at risk of hypercapnic respiratory failure due to conditions such as Chronic Obstructive Pulmonary Disease (COPD)
- Examine patient’s chest. If the patient is vomiting there is a risk of aspiration
- Chest X-ray if concerned about the patient’s ventilation or risk of aspiration. If the patient is unwell request a portable X-ray
- Obtain intravenous access by placing 2 large bore cannulae in the antecubital fossa. Take blood to check Full Blood Count (FBC), Urea and Electrolytes (U&Es), Liver Function Tests (LFTS), International Normalized Ratio (INR), Amylase, Glucose and Venous Blood Gas (VBG)
- Check Capillary Refill Time (CRT) - hold for five seconds and refilling should occur in 3 seconds
- Assess pulse rate, rhythm and character
- Abnormal rhythms should be managed immediately as in “Arrhythmias - Bradycardia” and “Arrhythmias - Tachycardia” Chapters in the “Medical Emergencies” section
- Monitor heart rate and blood pressure
- Listen to patient’s heart sounds
- Check urine output and consider catheterisation
- Intravenous (IV) fluids as required by clinical picture and balanced with patients’ risk of fluid overload. See more details in the “Circulation” Chapter in the “Response” Section under “Fluid Challenge”
- Check pupils are equal and reactive
- Assess Glasgow Coma Scale or ACVPU using the NEWS2 chart
- Check patient’s temperature and blood sugar
- Examine patient’s abdomen and legs
- Check sclera for jaundice and for liver flap (encephalopathy)
- Consider venous thromboembolism prophylaxis
- Call for senior help if not done already
Response
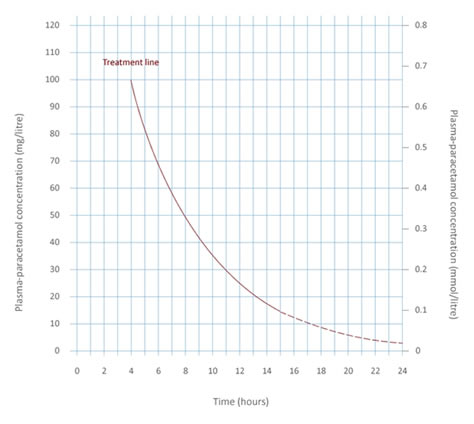
New treatment nomogram for paracetamol overdose (Reproduced with permission of MHRA under the terms of OGL v3.0).
- If < 1 hour of ingestion
- Give activated charcoal
- If < 4 hours of ingestion:
- Check bloods at 4 hours, including paracetamol levels
- Use paracetamol overdose treatment nomogram with paracetamol blood levels to decide if treatment needed with antidote (Intravenous N-Acetylcysteine)
- 4-8 hours
- Check paracetamol levels
- Use paracetamol overdose treatment nomogram with paracetamol blood levels to decide if treatment needed with antidote (Intravenous N-Acetylcysteine)
- If 8-16 hours
- Start treatment with antidote (Intravenous N-Acetylcysteine) and check bloods including paracetamol levels
- Use paracetamol overdose treatment nomogram with paracetamol blood levels to decide if treatment should be continued
- If level below the treatment line stop treatment
- If > 16 hours, a staggered overdose or signs of hepatotoxicity – Give full treatment – paracetamol levels not accurate
- 3 infusions over a total of 24 hours based on weight
- After treatment:
- Repeat bloods
- If bloods are normal N-Acetylcysteine can be stopped
- If bloods abnormal continue N-Acetylcysteine and discuss with the gastroenterology team
- Repeat bloods
- IV fluids
- Monitor for encephalopathy
- Referral
- Discuss with senior member of the team
- Contact critical care outreach team
- Consider referral to Gastroenterology team and Intensive Care Unit (ICU) if:
- Coagulopathic
- Renal failure
- Reduced GCS
- Patient may require referral to a transplant centre and should be discussed early in severe overdoses
- Once the patient is medically fit they need to be assessed by the psychiatric team to ensure they are safe to be discharged and have appropriate support