- “Any trauma to the head other than superficial injuries to the face” (NICE guidance CG 176)
If possible, ascertain if patient has:
- The mechanism of injury and if it was witnessed
- If following the injury, the patient has had:
- Amnesia
- Episodes of loss of consciousness
- Headache
- Seizures
- Vomiting
- If the patient has recently consumed alcohol
- If the patient has previously been:
- Diagnosed with a neurological condition
- Taking medication for a neurological condition
- If the patient has previously had any operations on their head or spine
- Any allergies
- Dizzy
- Focal neurological deficit for example:
- Blurred vision or double vision
- Difficulties walking
- Loss of power
- Slurred Speech
- Headache
- Nausea and Vomiting
- Photophobia
- Seizures
- Tinnitus
- Hypertensive
- Tachycardic or Bradycardic
- Signs of basal skull fracture
- Hemotympanum
- “Panda” eyes
- Cerebrospinal fluid leakage from ear or nose
- Battle’s sign (Bruising over the mastoid process)
- Confused
- Reduced Glasgow Coma Scale or ACVPU using the NEWS2 chart
- Cushing’s triad of signs is an indication of impending brain herniation. Cushing’s triad is made up of:
- Cheyne-Stokes breathing
- Hypertension
- Bradycardia
- If the patient has obtained the head injury through high-energy transfer mechanism then the patient’s cervical spine must be stabilised throughout the initial assessment of ABCDE
- Continue with ABCDE assessment
- Assess patient’s airway– call an anaesthetist if airway compromised
- Monitor oxygen saturations and respiratory rate
- If patient is hypoxic give Oxygen (O2) to achieve target saturations. Initially give 15 L/min via a reservoir mask if the patient is acutely unwell
- Target saturations:
- 94 - 98% for patients not at risk of hypercapnic respiratory failure
- 88 - 92% for patients at risk of hypercapnic respiratory failure due to conditions such as Chronic Obstructive Pulmonary Disease (COPD)
- Examine Patient’s chest. With reduced consciousness there is a risk of aspiration
- Arterial blood gas (ABG) if concerned about patient’s ventilation
- Obtain intravenous access by placing 2 large bore cannulae in the antecubital fossa. Take blood to check Full Blood Count (FBC), Urea and Electrolytes (U&Es), Liver Function Tests (LFTS), Clotting, Group and Save, and Venous Blood Gas (VBG)
- Check Capillary Refill Time (CRT) - hold for five seconds and refilling should occur in 3 seconds
- Assess pulse rate, rhythm and character
- Monitor heart rate and blood pressure
- Listen to patient’s heart sounds
- Check urine output and consider catheterisation
- Check pupils are equal and reactive
- Assess Glasgow Coma Scale (GCS). Ensure this is done carefully as it is important to notice and highlight to seniors any change in GCS
- Do full neurological examination of upper and lower limbs
- Do full cranial nerve examination
- Call for senior help
- Imaging
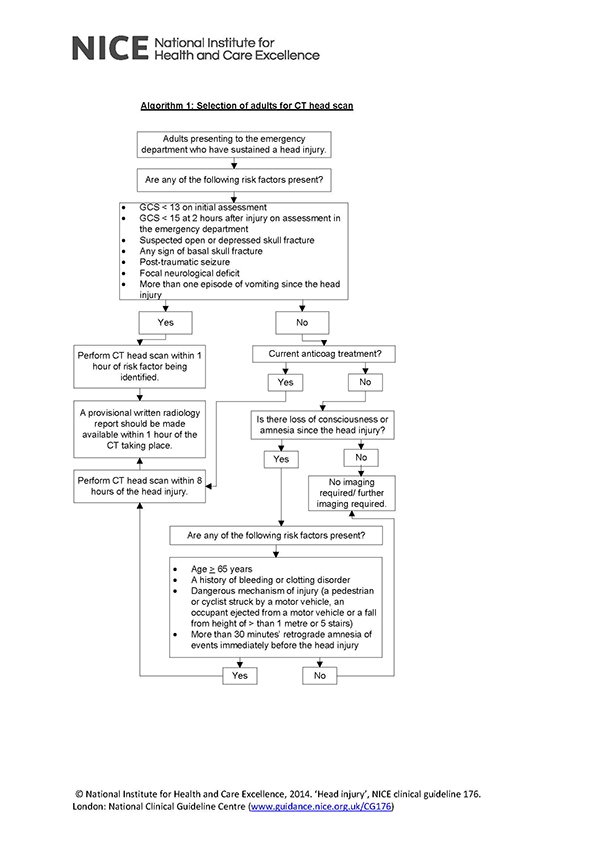
- See Algorithm 1 below: selection of adults for Computed Tomography (CT) head scan
- Potential diagnosis:
- Subdural haemorrhage
- Epidural haemorrhage
- Subarachnoid haemorrhage
- Intraparenchymal haemorrhage
- Skull fractures
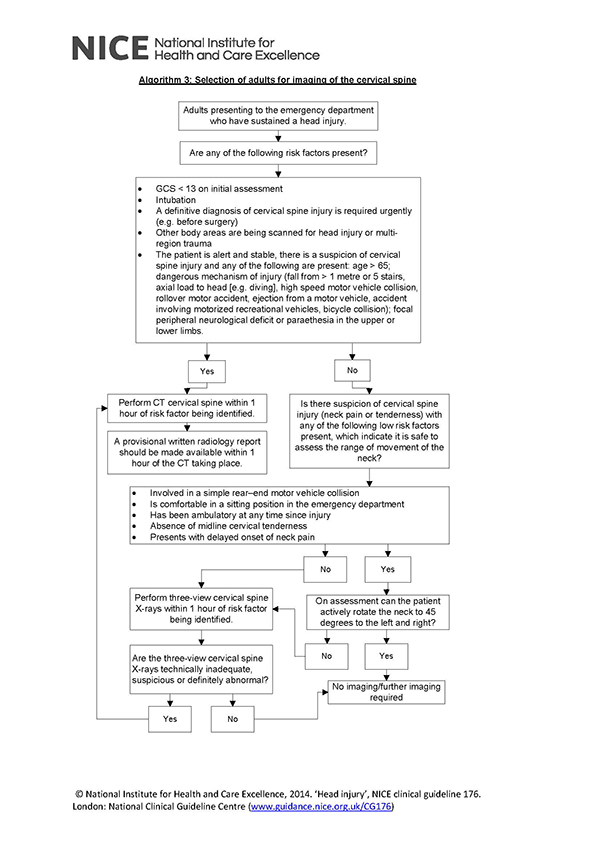
- Patients at risk of Cervical spine injury require Cervical spine X-rays unless they meet any of NICEs criteria for CT scan of the cervical spine (NICE guidance CG 176)
- Check patient’s temperature and blood sugar
- Examine patient’s abdomen and legs
- Ensure patient is in head up position (15-30o) to reduce intracranial pressure
Response
- Pharmacological
- Correction of any coagulopathies
- Following discussion with neurosurgery team patient may require:
- Prophylactic antiepileptics
- Mannitol
- Non-pharmacological management
- Surgical decompression with a craniotomy
- Discuss with senior member of the team
- Contact critical care outreach team
- Referral to neurosurgeons
- Consider referral to Intensive Care Unit (ICU) if:
- Patient requires transfer to centre with neurosurgical team
- Patient requires ventilator support
- Patient requires blood pressure support
- Deterioration of blood gases
- Ensure patient receives Occupational therapy and Physiotherapy review prior to discharge