ARRHYTHMIAS - BRADYCARDIA
Recognition
Sinus Bradycardia
- Definition
- Risk Factors
- Taking medicine known to cause bradycardia
- Age > 70 years
- Previous myocardial infarction
- Hypothyroidism
- Electrolyte disturbances
- Causes
- Sinus node dysfunction or conductive system dysfunction
- Intrinsic
- Inflammation
- Infection
- Degeneration due to age
- Congenital
- Extrinsic
- Toxins
- Medications
- Electrolyte imbalance
- History
- If possible, ascertain if patient has:
- Previous admissions with chest pain or cardiac conditions
- Been diagnosed with a cardiac condition
- Been taking medication for a cardiac condition
- Had any operations on their heart
- Any allergies
- General symptoms
- Shortness of breath (dyspnoea)
- Cyanosis
- Chest pain
- Fatigue
- Dizziness
- Reduced exercise tolerance
- Collapse
- General Signs
- Tachypnoea following pulmonary oedema from heart failure secondary to bradycardia
- Cool peripheries
- Bradycardia on palpation of pulse
- Hypotension
- Jugular venous distension from heart failure secondary to bradycardia
- Initial Assessment and Investigations
- ABCDE assessment
- Assess patient’s airway
- Monitor oxygen saturations and respiratory rate
- If patient is hypoxic give Oxygen (O2) to achieve target saturations. Initially give 15 L/min via a reservoir mask if the patient is acutely unwell
- Target saturations:
- 94-98% for patients not at risk of hypercapnic respiratory failure
- 88-92% for patients at risk of hypercapnic respiratory failure due to conditions such as Chronic Obstructive Pulmonary Disease (COPD)
- Examine patient’s chest
- Listening for:
- Bibasal crepitations
- Cardiac wheeze
- Arterial blood gas (ABG) if concerned about patient’s ventilation
- Chest X-ray if concerned about patient’s ventilation. If the patient is unwell request a portable X-ray
- Obtain intravenous access by placing 2 large bore cannulae in the antecubital fossa. Take blood to check Full Blood Count (FBC), Urea and Electrolytes (U&Es), Liver Function Tests (LFTs), Calcium, Magnesium, Glucose and Venous Blood Gas (VBG)
- Check Capillary Refill Time (CRT) - hold for five seconds and refilling should occur in 3 seconds
- Assess pulse rate, rhythm and character
- If no pulse present start advanced life support
- Monitor heart rate and blood pressure
- Listen to patient’s heart sounds
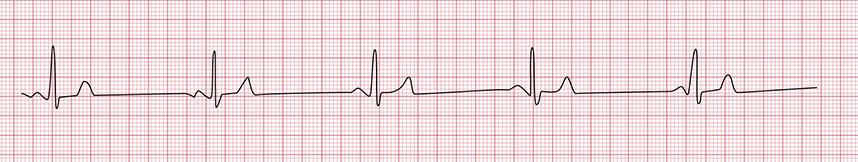
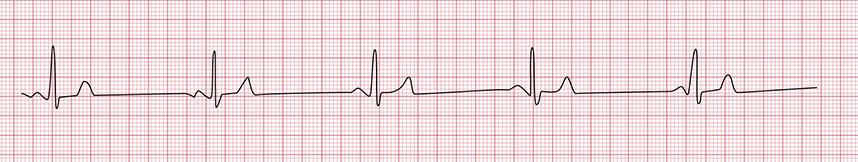
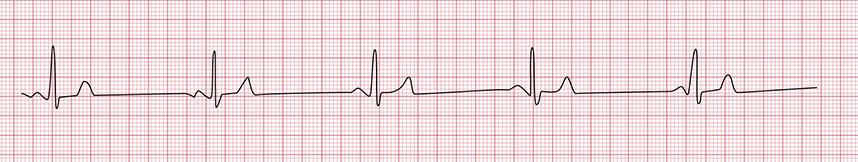
- 12 lead Electrocardiogram (ECG)
- Call for senior help
- Attach patient to cardiac monitor
- Identify underlying cause and treat
- Identify adverse features:
- Shock
- Syncope
- Myocardial ischaemia
- Heart failure
- Check patient’s urine output and consider catheterisation
- Check pupils are equal and reactive
- Assess Glasgow Coma Scale or ACVPU using the NEWS2 chart
- Check patient’s temperature and blood sugar
- Examine patient’s abdomen and legs
- Consider venous thromboembolism prophylaxis
Response
- Immediate management
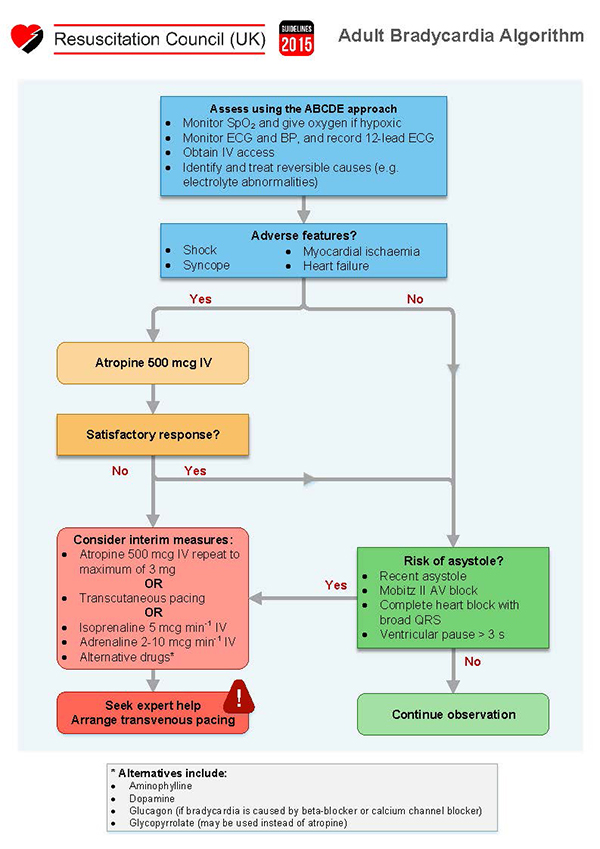
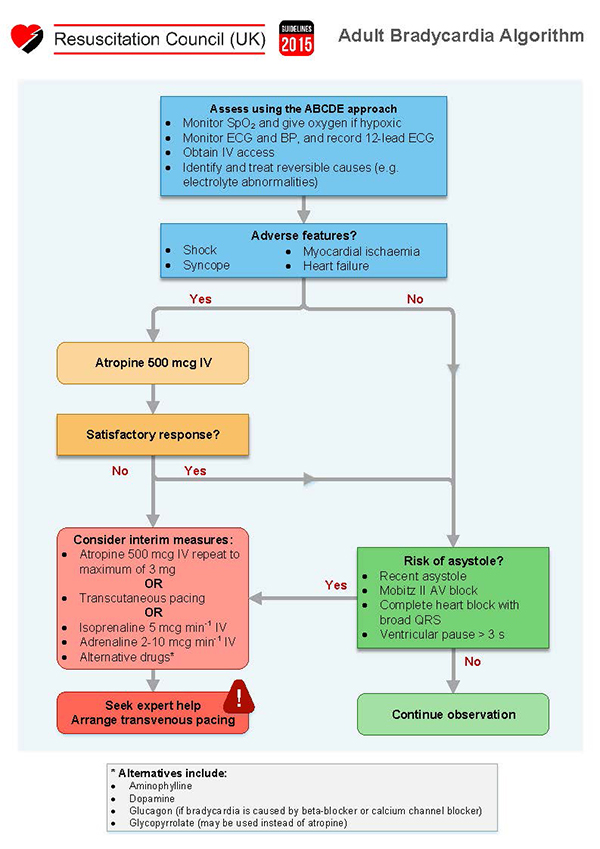
Bradycardia algorithm
- Referrals
- Discuss with senior member of the team
- Contact critical care outreach team
- Referral to cardiologists
- Referral to anaesthetists if cardioversion is required
- Consider referral to Intensive Care Unit (ICU) if:
- Failure to respond to medical management
- Patient requires ventilator support
- Patient requires blood pressure support
- Deterioration of blood gas following medical management
- Future management
- Review by cardiologists regarding future management