- “Anaphylaxis is a severe, life-threatening, generalised or systemic hypersensitivity reaction.” (RESUS.org).
- Asthma
- Atopy
- Exposure to common sensitizer
- Previous anaphylaxis
- Insect stings
- Latex
- Food
- Nuts
- Milk
- Egg
- Fish
- Shellfish
- Penicillin
- Angiotensin Converting Enzyme inhibitors (ACEi)
- If possible, ascertain if patient has:
- Previous admissions with anaphylaxis
- Any known allergies
- Any admissions to Intensive Care Unit (ITU) with anaphylaxis
- Any allergies
- Shortness of breath (dyspnoea)
- Cyanosis
- Angio-oedema
- Rhinitis
- Clammy
- Abdominal pain
- Dizziness
- Collapse
- Urticaria
- Diarrhoea
- Low oxygen saturations
- Tachypnoea
- Wheeze
- Stridor
- Pale
- Cool peripheries
- Delayed capillary refill time
- Reduced skin turgor
- Dry mucous membranes
- Hypotensive
- Tachycardic
- Decreased urine output
- ABCDE assessment
- Assess patient’s airway – call an anaesthetist if airway compromised
- Assess patients face for swelling
- Monitor oxygen saturations and respiratory rate
- Give 15 L/min via a reservoir mask
- Call for senior help
- Once anaphylaxis recognised give immediate management and remove the antigen if identified
- Arterial blood gas (ABG) but this is not a priority
- Examine patient’s chest
- Listening for:
- Wheeze
- Listening for:
- Obtain intravenous access by placing 2 large bore cannulae in the antecubital fossa. Take blood to check Full Blood Count (FBC), Urea and Electrolytes (U&Es), Liver Function Tests (LFTs), Mast Cell Tryptase, Calcium and Glucose
- Check Capillary Refill Time (CRT) - hold for five seconds and refilling should occur in 3 seconds
- Assess pulse rate, rhythm and character
- If no pulse present start advanced life support
- Monitor heart rate and blood pressure
- Raise the legs to help restore circulation
- Listen to patient’s heart sounds
- Intravenous (IV) fluid bolus of 0.9% sodium chloride 250-500 ml over 10-15 mins as described in management.
- See more details in the “Circulation” Chapter in the “Response” Section under “Fluid Challenge.”
- Repeat as required to maintain blood pressure
- 12 lead Electrocardiogram (ECG)
- Consider cardiac monitoring
- Remove the antigen if identified and not done already
- Check pupils are equal and reactive
- Assess Glasgow Coma Scale or ACVPU using the NEWS2 chart
- Check patient’s temperature and blood sugar
- Examine patient’s abdomen and legs for rash
- Consider venous thromboembolism prophylaxis
Response
- Follow RESUS guidelines
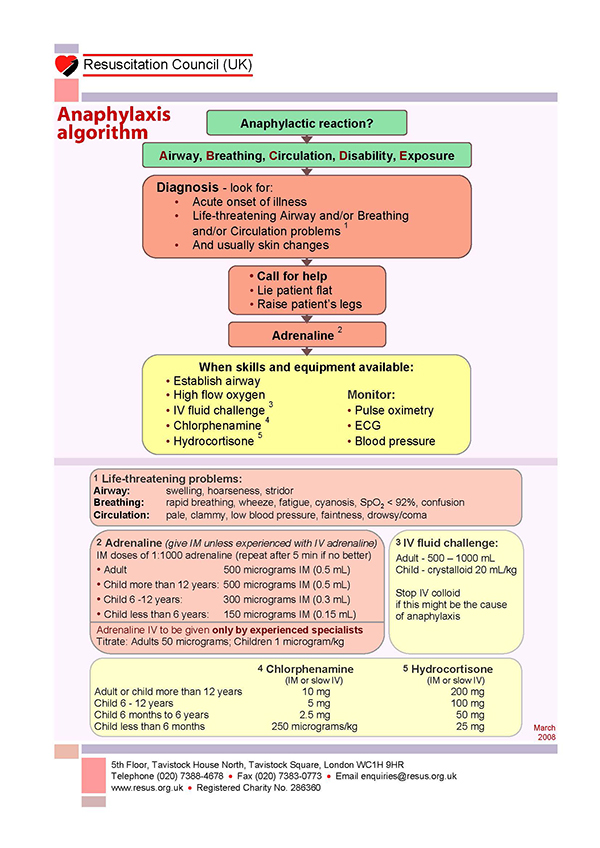
Anaphylaxis algorithm
- Discuss with senior member of the team
- Contact critical care outreach team
- Consider referral to Intensive Care Unit (ICU) if:
- Failure to respond to medical management
- Patient requires ventilator support
- Patient requires blood pressure support
- Deterioration of blood gas following medical management
- A second sample of mast cell tryptase should be taken 1 - 2 hours post event
- Patient should be observed for 6 -12 hours post event in case of biphasic reaction
- Patient should be referred to specialist allergy service