C
RECOGNITION
Life threatening problems with airway or breathing should be
treated first before assessment of the circulation. Some breathing problems
such as tension pneumothorax or PE will cause circulatory collapse (obstructive
shock) and will require urgent treatment as a priority.
Assessment of circulation
- Feel the patient’s peripheries – cool and clammy or warm and pink?
- What is the capillary refill time?
- Feel a peripheral pulse – unable to feel or weak and thready?
- What is the pulse rate?
- Is the oxygen saturations probe able to pick up a pulse?
- What is the blood pressure?
- Look for signs of poor end organ perfusion
- Agitation
- Reduced consciousness
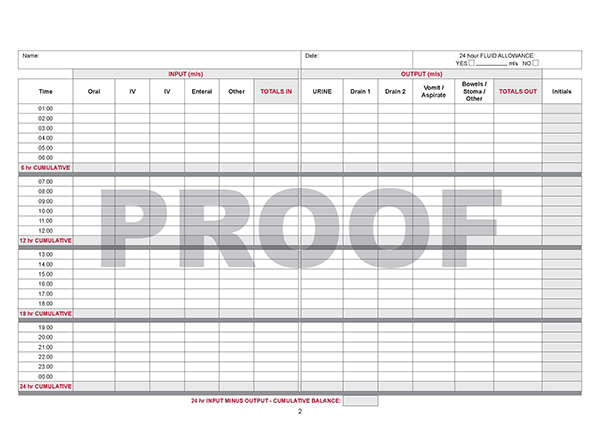
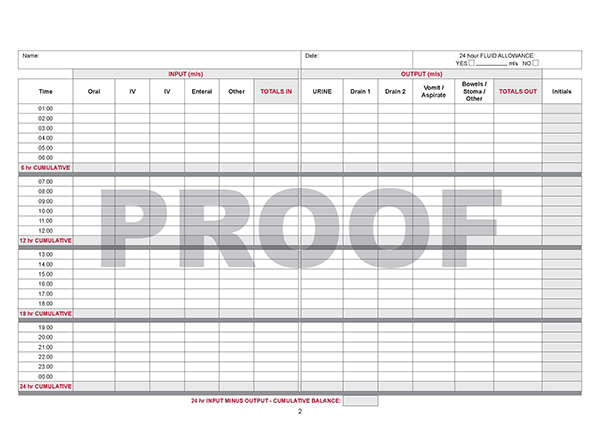
- Urine output < 0.5 mls/kg/hr (Look at the fluid balance charts)
- Is there a metabolic/lactic acidosis? (Perform an arterial blood gas)
Fluid management
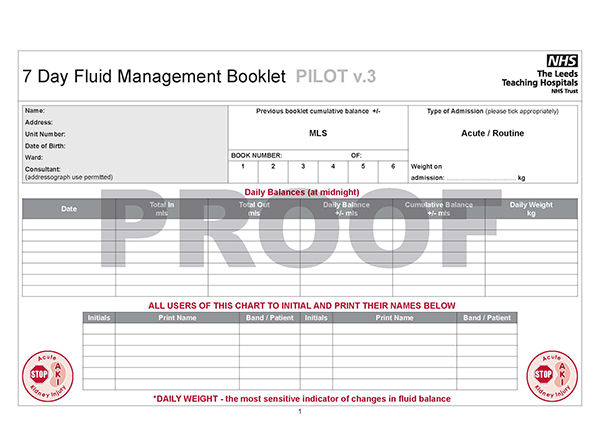
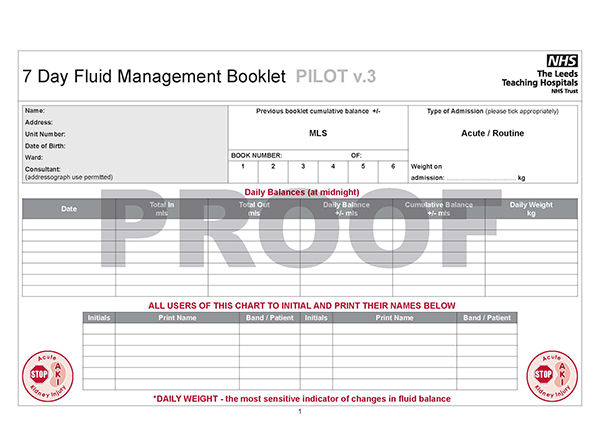
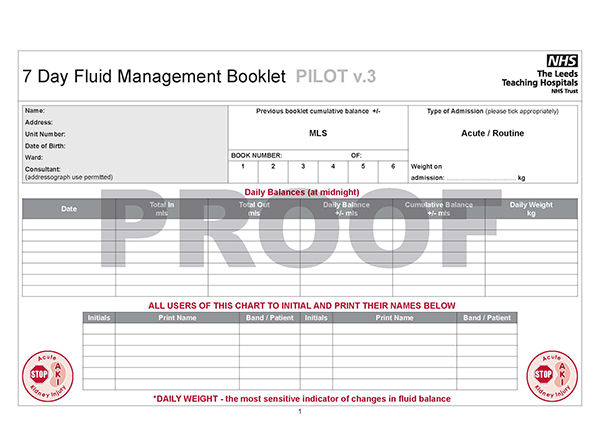
Fluid balance chart
Assessment of volume status:
Assessment of the volume status would include the evaluation of the following:
- Capillary refill time (< 2 s)
- Pulse rate (beta blockers/diltiazem prevent tachycardia)
- Blood pressure (lying and standing unless hypotensive)
- Jugular venous pressure
- Skin turgor (over clavicle)
- Heart sounds (gallop rhythmn - hypervolaemia)
- Lungs (pulmonary oedema)
- Oedema (peripheral/sacral)
- Urine output
- Trends in weight change to assess water balance
Video: Circulation Assessment.
Signs of hypovolaemia
- Cool, clammy peripheries (unless septic)
- Capillary refill time (CRT) > 2 seconds, peripherally
- Reduced skin turgor
- Postural drop in blood pressure (20 mmHg)
- Jugular venous pressure (JVP) reduced
- Dry mucous membranes
- Tachycardia (100 beats/min)
- Decreased urine output (< 0.5 ml/kg/hour) or decreasing trend
Signs of Hypervolaemia
- Short of breath
- Reduced saturations
- Tachypnoeic
- Fine inspiratory crackles at lung bases on auscultation
- Tachycardia or Bradycardia
- Jugular venous pressure (JVP) raised
- Third heart sound
- Cardiac murmur
- Peripheral oedema/ Dependent oedema
What is the aetiology?
Determining the underlying cause
of circulatory failure is important to direct further management of the patient.
- You have established the patient has evidence of poor tissue
perfusion and therefore shock.
- Does the patient have signs of hypovolaemia?
- What is the cause of the hypovolaemia? (e.g. bleeding, inadequate fluid
resuscitation, inappropriate diuretic use). A thorough review of the fluid
balance charts, blood results and drug charts will be needed.
- Is there evidence of sepsis? (e.g. pyrexia, source of infection, warm to
touch)
- Is there evidence of a cardiogenic cause? (e.g. raised JVP, pulmonary oedema,
ECG changes consistent with myocardial ischaemia, arrhythmias)