In order to fully understand the pathophysiology of the different types of shock and cardiovascular system dysfunction, an understanding of basic cardiovascular physiology and terminology is required.
The cardiovascular system comprises the heart, blood vessels and blood.
Circulation refers to the circulating fluid (blood), within the blood vessels and tissues, which deliver nutrients and removes waste products in order to maintain homeostasis. Oxygen (O2) is delivered from the lungs to the circulation and then transported to the tissues, and carbon dioxide (CO2) is removed.
The function of the heart is to pump blood around the body. The left ventricle contracts during systole and ejects oxygenated blood through the aortic valve into the aorta which then travels via the arteries and capillaries to the tissues.
The volume of blood ejected by the ventricle per heartbeat is the stroke volume (SV), which is normally 70-80 mls for a 70 kg man at rest. Stroke volume varies with the force of ventricular contraction (myocardial contractility), the volume of blood in the ventricle at the end of diastole (preload) and the outflow resistance (afterload).
Preload refers to the volume of blood returning to the right or left ventricle during diastole. It can be thought of as a measure of ‘filling’. It will drop if a patient is under-filled due to dehydration or bleeding. It will increase following a fluid challenge, as this will increase circulating volume and therefore the volume of blood returning to the heart with each beat.
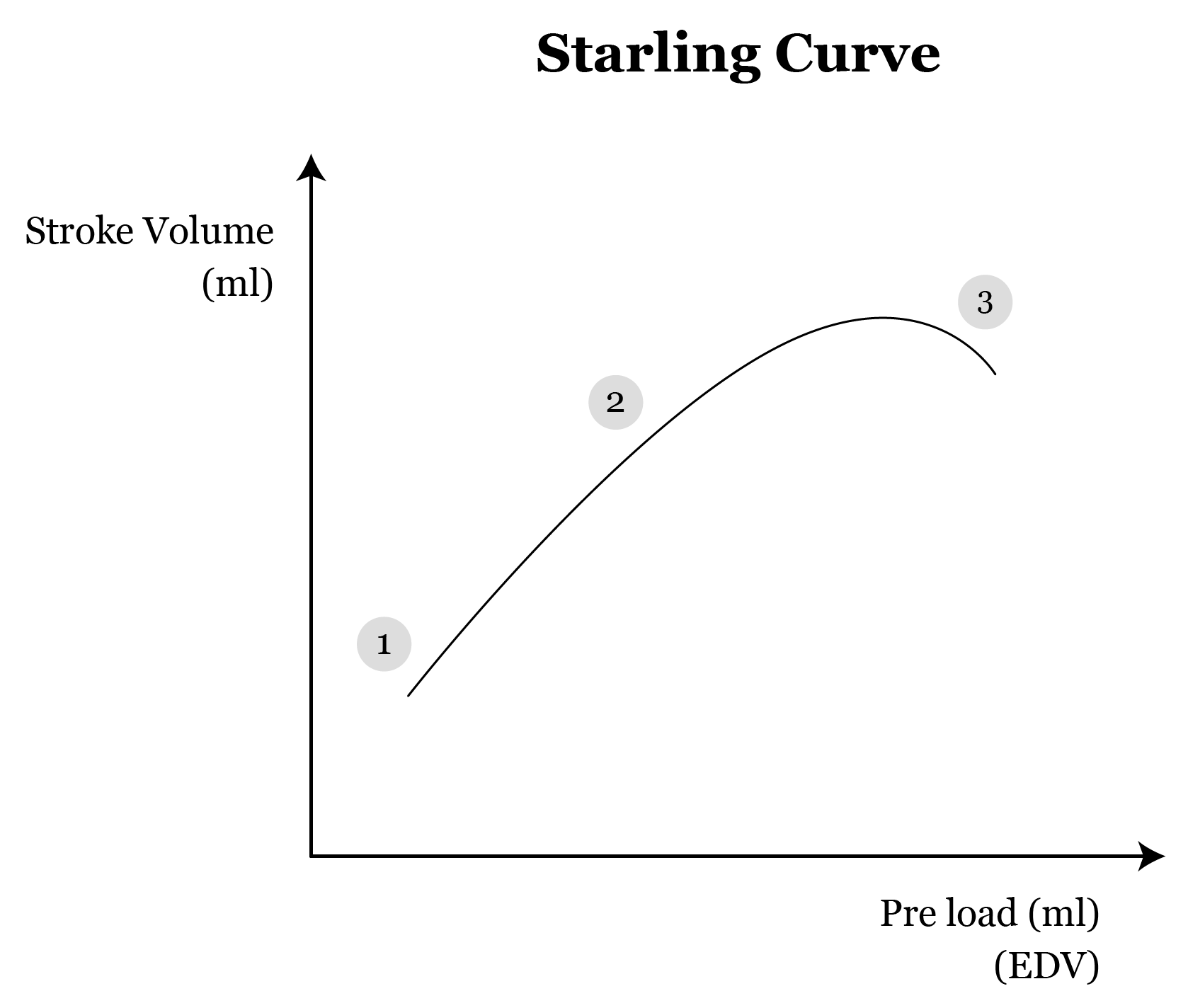
Starling’s law of the heart shows that there is a predictable relationship between the preload and the stroke volume produced. It shows that the force of myocardial contraction produced is proportional to the initial myocardial fibre length within a normal physiological range. This means that the larger the volume of blood returning to the ventricle per heartbeat, the larger the end diastolic ventricular volume, the bigger the stretch of the myocardial fibres, the bigger the force of ventricular contraction and the bigger the stroke volume. There is a point, however, at which the myocardial fibres become overstretched, when the preload is too great, and at this point the myocardial fibres do not work effectively and the force of contraction reduces.
Starling’s law of the heart is represented in Frank-Starling’s curve (shown below).
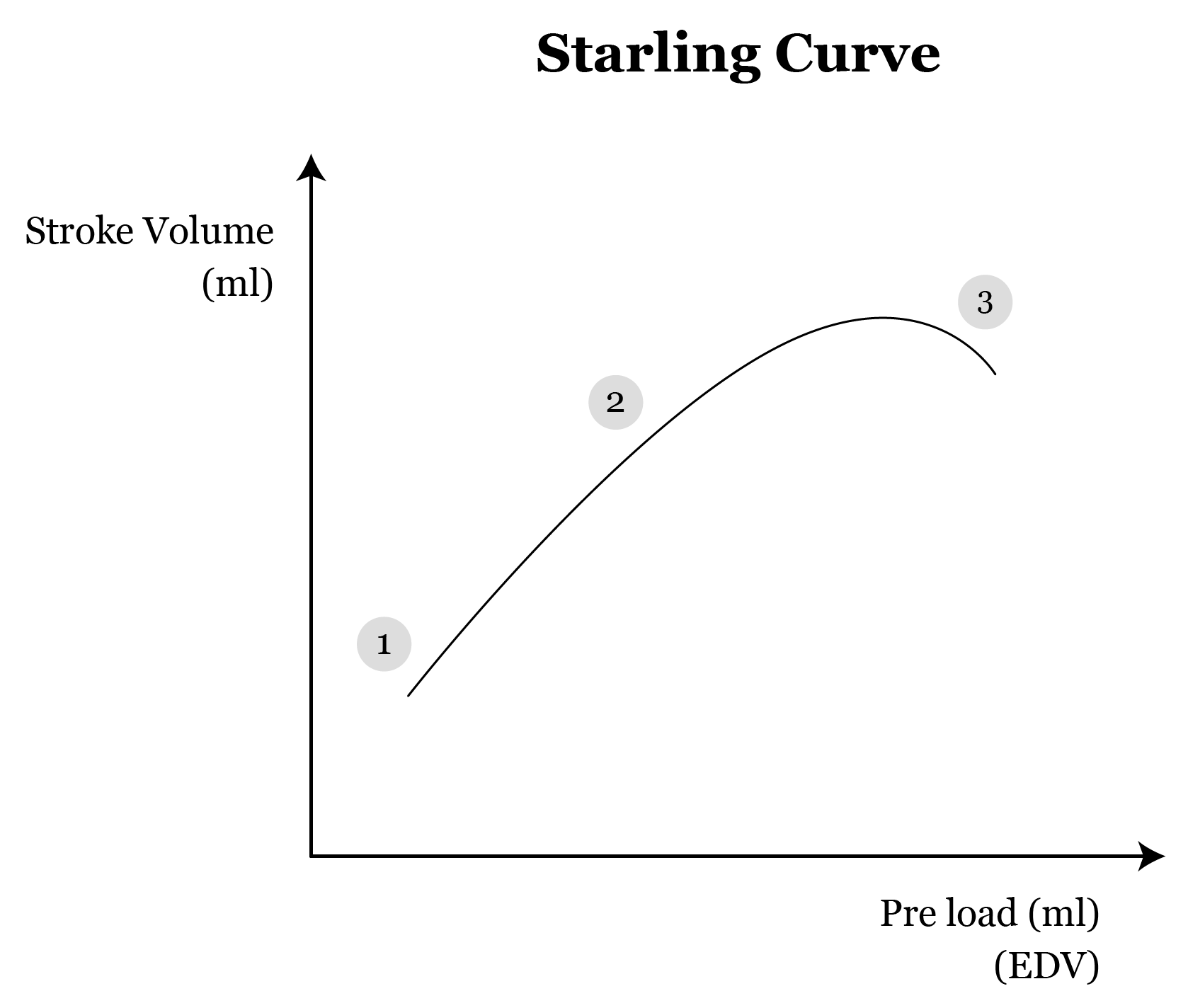
When a patient has heart failure caused by impairment of contraction of the left ventricle, the curve is displaced downwards. This means that at any given end diastolic volume and therefore preload, the produced stroke volume will be lower. In some patients the impairment of ventricular contraction and therefore decreased stroke volume, will result in back pressure that is larger than the hydrostatic forces of the pulmonary venous system. This results in the development of pulmonary oedema.
Myocardial contractility is the force with which the myocardium contracts which is a major determinant of stroke volume. Contractility is increased by various factors such as increasing preload, increased sympathetic nervous system activity (stress response) and inotropic drugs (adrenaline). Contractility is reduced by low preload (hypovolaemia), cardiac disorder (e.g. ischaemic heart disease, heart failure, arrhythmias), hypoxia, hypercapnoea, acidosis and electrolyte disturbances.
Afterload is the ‘load’ against which the heart must contract to eject blood. It is the tension in the left ventricle during systole. Increased afterload results in increased myocardial work and a decreased stroke volume. One component of afterload is the systemic vascular resistance.
Systemic vascular resistance (SVR) or peripheral vascular resistance (PVR) is the resistance of the arteries and arterioles to the flow of blood pumped out of the heart. Small changes in the diameter of arterioles produce large changes in the SVR and therefore afterload. SVR is directly proportional to blood pressure and a drop in SVR leads to a drop in the arterial blood pressure if all other factors remain constant. SVR increases with age leading to hypertension.
Cardiac output (CO) is the volume of blood pumped by the heart per minute. It is a product of the stroke volume (SV) and heart rate (HR). It is normally about 5 L/min in a fit 70 kg man at rest.
CO is therefore increased by increasing heart rate, increasing preload, increasing cardiac contractility and decreasing afterload.
The circulation is driven by blood pressure. Too high a pressure would lead to damage to vessel walls and haemorrhage while too low a pressure fails to adequately perfuse tissues leading to ischaemia and potentially end organ damage.
The mean arterial pressure (MAP) is proportional to the CO and the SVR.
MAP = CO × SVR
Thus, arterial pressure varies with changes in cardiac output (stroke volume and heart rate) and vascular resistance.
MAP= diastolic pressure + 1/3(Systolic pressure-diastolic pressure)
Mean arterial pressure may also be calculated from the diastolic pressure and systolic pressure