
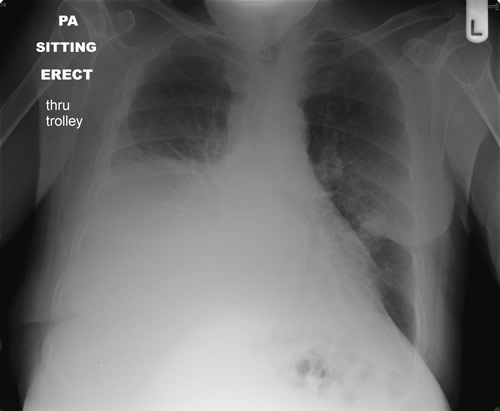
This X-ray of a patient with COPD shows hyperinflation, flattening of the hemidiaphragms and a small right pleural effusion (blunting of the right costophrenic angle).
Video: Peak Flow Meter.
Asthma causes inflammation and bronchoconstriction of the airways leading to a narrowed bronchial lumen. A reduced peak expiratory flow rate (PEFR) is usually present. Acute exacerbations of asthma present with respiratory distress, tachypnoea, tachycardia, and widespread wheeze.
Chest X-ray findings:
Treatment:
ABGS are required to guide further management.
Information on tension pneumothorax can be found in the medical emergencies section of this eBook.

This X-ray of a patient with COPD shows hyperinflation, flattening of the hemidiaphragms and a small right pleural effusion (blunting of the right costophrenic angle).
A combination of chronic bronchitis and emphysema are almost always associated with a history of smoking. This is a chronic disease but is associated with frequent exacerbations that often require hospitalisation. These patients are at risk of Type 2 respiratory failure if treated with uncontrolled oxygen therapy (loss of hypoxic drive).
Chest X-ray findings:
Treatment:
ABGs are required to guide further management - if not improving the patient may need further intravenous medications and/or non-invasive ventilation. These patients can deteriorate rapidly and require early expert input.
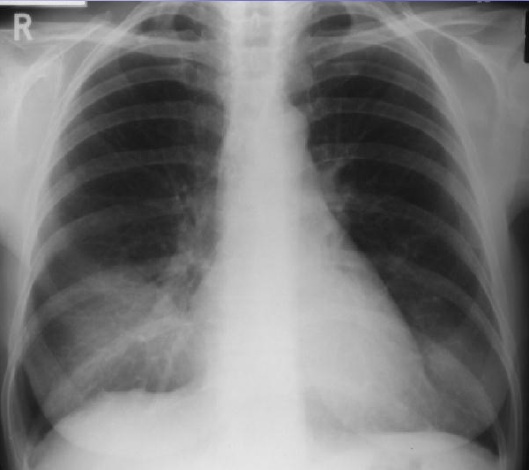
There is a right-sided pleural effusion. This is evident from the homogenous dense shadowing, loss of the right costo-phrenic angle and meniscus (implying the fluid is in the pleural cavity rather than consolidation within the lung itself).
A pleural effusion is accumulation of fluid in the pleural space.
It can either be a transudate or exudate. A pleural effusion usually has an underlying cause, such as pneumonia (para-pneumonic effusion), so further investigation will be necessary. Clinical findings include reduced air entry on the affected side and a ‘stony dullness’ to percussion.
Chest X-ray findings:
The presence of costophrenic blunting on a chest X-ray indicates that at least 500ml of fluid is present in the chest cavity. It is always safer to confirm the presence of fluid with an ultrasound before drainage.
ABGS are required to guide further management.
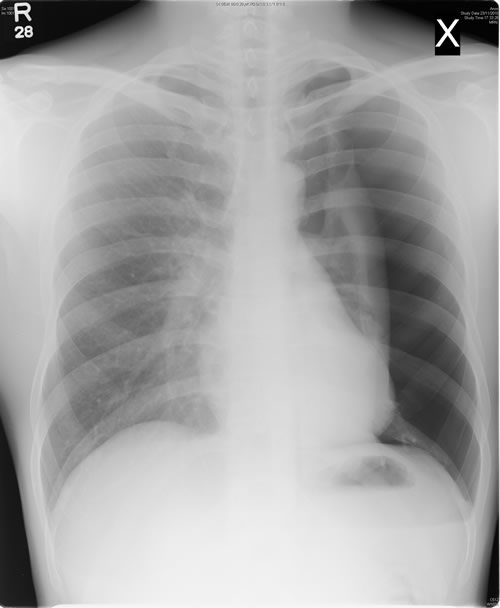
Right lower zone air space shadowing with loss of the right heart border consistent with a right middle lobe pneumonia.
Pneumonia is secondary to infection and inflammation of the lung parenchyma and may result in the appearances of consolidation on the chest X-ray. It can be localised or widespread. Clinical findings include reduced air entry on the affected side, crackles and bronchial breathing. The patient is likely to have a pyrexia and raised inflammatory markers.
Chest X-ray findings:
Treatment:
ABGS are required to guide further management.
This chest X-ray shows a large left sided pneumothorax. The lung edge is clearly visible with no lung markings peripherally. There is no significant mediastinal shift.
A pneumothorax is air in the pleural space. It can be spontaneous, secondary to respiratory disease or traumatic (e.g. stabbings, gun shot wounds, road traffic collisions). A serious consequence of developing a pneumothorax is the development of a tension pneumothorax. This may result in compression of the lung and mediastinum, reduced cardiac filling leading to cardiac arrest. Typically a pneumothorax comes under tension when there is a one-way valve formed, allowing air into the pleural space on inspiration but not out again on expiration. The clinical symptoms and signs of pneumothorax can be vague and inconclusive, and confirmation with imaging is usually required.
Chest X-ray findings:
Treatment:
ABGS are required to guide further management.
Information on tension pneumothorax can be found in the medical emergencies section of this eBook.
Emboli generated from deep vein thrombosis can travel to the pulmonary vasculature. Massive pulmonary emboli (PE) can block blood flow very proximally in the vasculature leading to obstructive shock, haemodynamic compromise (raised heart rate (HR) and low blood pressure (BP)) and death. Smaller emboli may cause sudden onset pleuritic chest pain, haemoptysis and shortness of breath.
Clinical examination is often unremarkable but observations may include a raised respiratory rate, sinus tachycardia and low oxygen saturations. The gold standard diagnostic tool for PE is computed tomography pulmonary angiogram (CTPA).
Chest X-ray findings:
Treatment:
Further guidelines can be found on the British Thoracic Society website.
ABGS are required to guide further management.
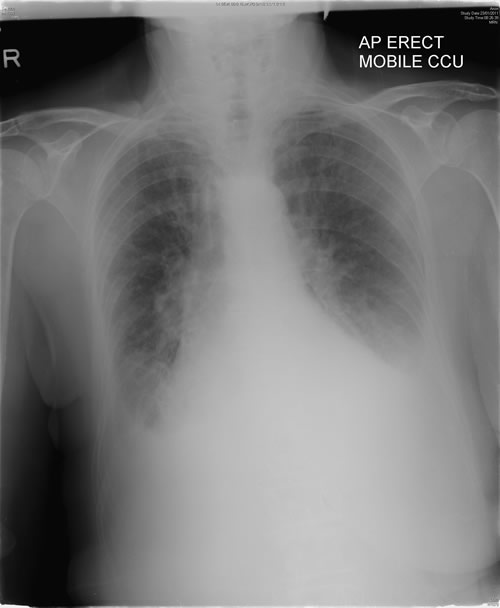
This X-ray shows perihilar haziness, peribronchial cuffing, upper lobe venous blood diversion and bilateral pleural effusions in keeping with decompensated heart failure.
Pulmonary oedema is fluid accumulation in the alveoli. It can be cardiogenic or non-cardiogenic. The most common cause of severe pulmonary oedema is acute left ventricular failure. The clinical findings include hypoxia, end inspiratory crackles, which may be localised or widespread, wheeze and respiratory distress.
Chest X-ray findings may include:
Treatment includes:
ABGS are required to guide further management.
Information on pulmonary oedema can be found in the medical emergencies section of this eBook.