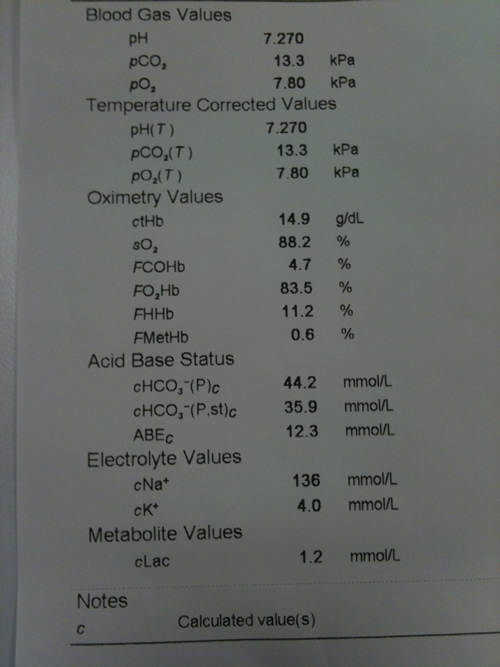
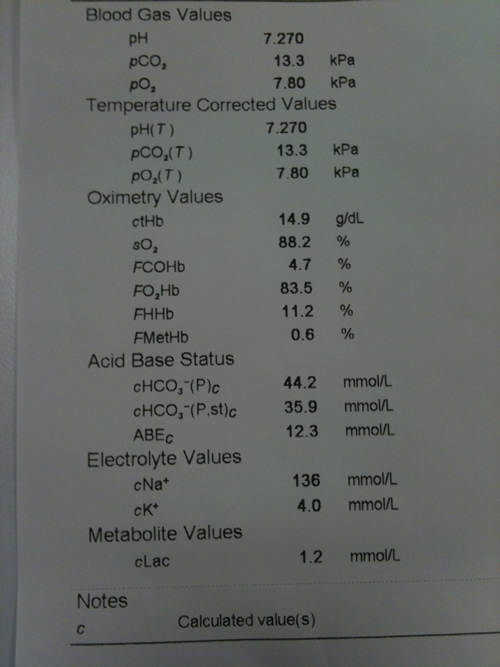
ABG paper print out
Video: Arterial blood gas sampling.

An ABG is obtained from an artery – usually the radial artery using a blood gas syringe and needle. Details of this procedure can be found in the University of Leeds clinical eBook (http://clinicalskills.leeds.ac.uk/). Interpreting the results of an ABG is important to determine the cause and severity of acute patient deterioration.”
There are four key components to analysing an ABG
The normal range of pH is 7.35-7.45. Acidosis is defined as a pH <7.35 and can be either metabolic or respiratory in origin. Alkalosis is defined as a pH >7.45 and can be either metabolic or respiratory in origin. Sometimes an acidosis or alkalosis can be due to more than one process and is termed ‘ mixed’. This text will be restricted to describing the simple acid/base disturbances which are secondary to one process.
A respiratory acidosis is characterised by a pH <7.35 with an elevated level of carbon dioxide (CO2). Carbon dioxide is converted into acid in the blood stream and so raised levels will result in an acidosis. This can occur acutely due to respiratory depression secondary to drugs or neurological damage, respiratory muscle weakness, chest injury or acute airways obstruction.
Low levels of CO2 are found in conditions where the patient is hyperventilating (e.g. pulmonary embolism, neurological insult, anxiety) and will result in an alkalosis. A respiratory alkalosis is characterised by a pH >7.45 with a reduced level of CO2.
A metabolic acidosis is characterised by a pH <7.35 with a reduced bicarbonate (HCO3- ) level. Bicarbonate acts like a base in the blood and mops up excess hydrogen ions (H+) resulting in a reduced bicarbonate level. There are four major causes of a metabolic acidosis including ketoacidosis, lactic acidosis, poisonings or advanced acute or chronic kidney disease.
A metabolic alkalosis is characterised by a pH >7.45 with a high bicarbonate level and can occur in association with fluid depletion (for example vomiting) or hyperaldosteronism excess.
When an acid/base disturbance occurs the body will try to compensate for it to try and normalise the pH. Compensation occurs over a variable period of time depending on the cause. Full compensation has occurred when the pH has returned to within normal limits. Partial compensation implies that the pH is still abnormal but a change has occurred to try and normalise it.
Respiratory compensation happens quickly (minutes to hours) by increasing or decreasing the respiratory rate and therefore the amount of CO2 removed or retained. Metabolic compensation occurs via the kidneys by increasing the regeneration of HCO3- or removal of H+ and may take hours to days to occur.
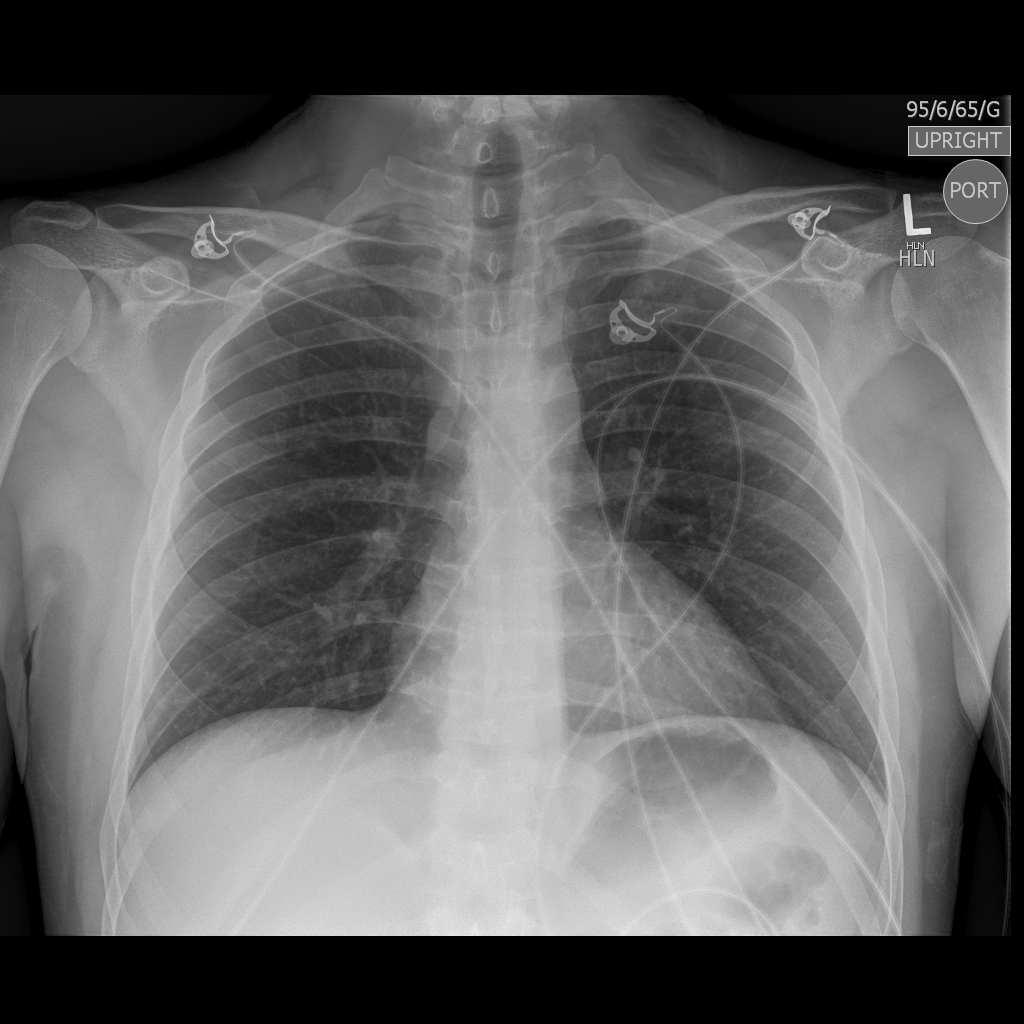
This is an adequate portable plain AP chest X-ray. Bones and soft tissues look normal. ECG lines are visible attached externally to the patient. The trachea is central, lung fields are clear, costophrenic angles are visible. The cardiac shadow does not look enlarged (even considering it is an AP film). There is no free air below the diaphragm and a normal gastric bubble is visible below the left hemi-diaphragm.
A plain chest X-ray (CXR) is a valuable investigation in the acutely ill patient. If the patient is unstable, do not transfer them to the radiology department but request a portable X-ray on the ward. CXR signs tend to lag behind clinical signs so it is not a substitute for thorough clinical examination. It is important to have a system when assessing a chest X-ray. One example that is commonly used is based on an ABCDE mnemonic.
The British Thoracic Society Guidelines published in 2017 outlines emergency oxygen use in adult patients, https://www.brit-thoracic.org.uk/quality-improvement/guidelines/emergency-oxygen/. These were updated in 2019.
The underlying principle is that hypoxia is dangerous and needs to be treated assertively. A reservoir bag mask with 15 L/min O2 running is the treatment of choice in an acutely ill -patient.
In an improving patient with previously normal, healthy lungs, O2 therapy should be titrated to target saturations of 94-98% via pulse oximetry using a variety of O2 delivery devices.
There are a subset of patients who are at risk of type 2 respiratory failure and CO2 retention, especially if exposed to uncontrolled O2 therapy. This can occur in a percentage of patients with Chronic Obstructive Pulmonary Disease (COPD). This leads to a respiratory acidosis. There are several theories as to why this happens which includes the impairment of hypoxia-induced respiratory drive.
This subset of patients requires controlled O2 which can be given most effectively via a Venturi mask which provides a fixed concentration of O2 at a given flow rate. Venturi masks come in different colours denoting the different inspired O2 concentration (24%, 28%, 35%, 40%, 60%). At 24%, the hole through which the jet of O2 is delivered is much smaller than at 60%. Forcing a jet of O2 through a small hole causes a low-pressure area within the mask, which causes surrounding air to be dragged in, thus diluting the O2 causing a lower inspired O2 concentration for the patient. As the percentage increases, less air is drawn into the mask causing a higher inspired O2 concentration. The Venturi masks are flow dependent, and it is essential to use the recommended flow rate to get the required percentage of inspired oxygen.


Hypoxia can rapidly lead to hypoxic brain injury, respiratory and cardiac arrest and death within minutes. Therefore never allow a patient to become hypoxic in order to attempt to control rising CO2 levels. Treat hypoxia in a controlled manner and if the CO2 continues to rise, get help.
In the subset of patients who are at risk of type 2 respiratory failure and CO2 retention, especially if exposed to uncontrolled O2 therapy, it is important to titrate O2 saturations to 88-92%, using a venture mask. Once within the target O2 saturation range using pulse oximetry, arterial blood gas sampling must be used to ensure CO2 levels are within normal limits.
Patients with Chronic Obstructive Pulmonary Disease (COPD) have chronically raised CO2 levels resulting in a chronic respiratory acidosis, and rely on a hypoxic drive mechanism to maintain their ventilation. This may be indicated by a compensated respiratory acidosis, as reflected by a normal pH, high PCO2 and high HCO3-.
It is essential to monitor the pH, and if the patient is acidaemic with rising CO2, non-invasive ventilation and/or escalation of care may be required.
Oxygen Delivery device |
Percentage Oxygen Delivered (%) |
Flow rate (L/min) |
Nasal Canula |
24-30 |
1-4 |
Hudson mask |
30-40 |
5-10 |
Venturi mask: Blue White Yellow Red Green |
24 28 35 40 60 |
2-4 4-6 8-10 10-12 12-15 |
Reservoir mask |
85-90 |
15 |